Acquisition Protocols
General Comments
- Standard field of view or smaller (15 - 13 inches) is preferred - A smaller field is preferred (why?)
- Crystal = 3/8" NaI(Tl)
- Consider the energy gamma being emitted by the patient and crystal thickness
- The crystal on a 3/8" camera is specifically designed for 140 keV gammas
- How does this play into the 201Tl energy spectrum?
- Parallel hole collimator
- 201Tl = GAP or HR
- 99mTc-cardiac agent = HR or ultra HR
- Consider the difference between using these two types of collimators
- Which one will have more scatter counts?
- Other types of specialty collimators can be considered in cardiac imaging
- Slant hole collimator can acquire multiple projections while being placed at one specific location
- This acquisition can be completed by rearranging the septa into specific angles. We will discuss in greater detail in our instrumentation course (CLRS 322)
- When should thallium scan be done?
- While I thought that thallium is something of the "past" the issue that confronts us, from time to time is the shortage of 99mTc. Whenever this issue does present itself, thallium becomes the viable alternative
- Second point to consider, which is not done in the Richmond area, is a dual isotope procedure which popular in other areas of the US. This is where 201Tl is used as the resting portion and 99mTc-cardiac agent is applied at stress
- A third point to make is the need to evaluate myocardial viability, if this data is needed one may consider thallium viability study
- Energy Peaks
- 201Tl = (69 - 83) keV (47%), 135 keV (3%) and 167 keV (10%) - usually the peak is set around 71 keV
- T1/2 3.04 days
- Data sheet
- 99mTc = 140 keV (20%)
- Matrix
- Planar imaging should be set at 128 x 128
- SPECT can be 64 x 64 or 128 x 128
- In general, most if not all of your SPECT imaging should be set at 64 x 64. This issue relates to count density and statistical noise. This concept will be covered in Nuclear Medicine Physics
- Radiation Dosimetry of the different cardiac agents to the heart wall
- 4 mCi of 201Tl = 20 rads
- 40 mCi of 99mTc-sestamibi = 0.67 rads
- 40 mCi of 99mTc-tetrfosmin = 0.7 rads
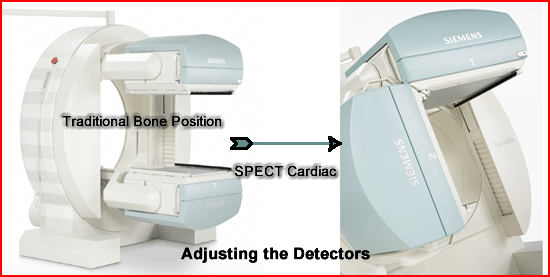
- Types of cameras - detector head positioning
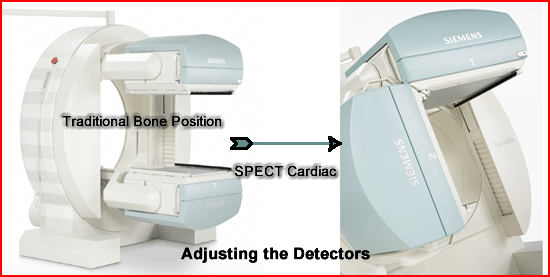
- The traditional approach is with the use of a single or dual headed system. In the typical two-headed system the detectors are brought around to a 90 degree angle
- Siemens Symbia Evo FOV is 53.3 x 38.7 cm
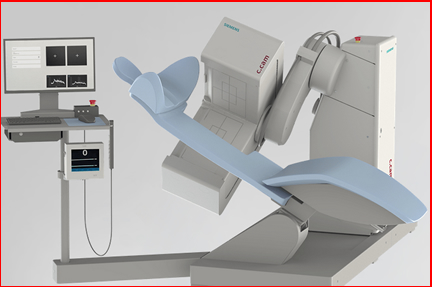
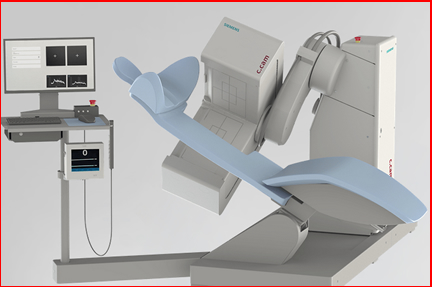
- Dedicated SPECT cardiac has the two-headed system fused to together at a 90 degree angle. This camera is from Siemens Medical and is called C.Cam
- Siemens C.Cam FOV is 37 x 21.4 cm
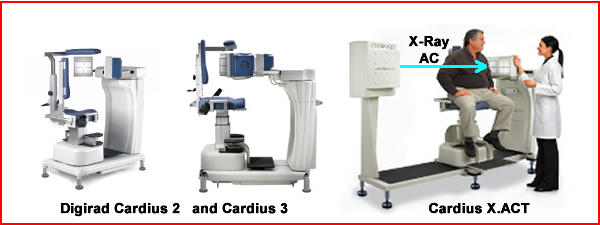
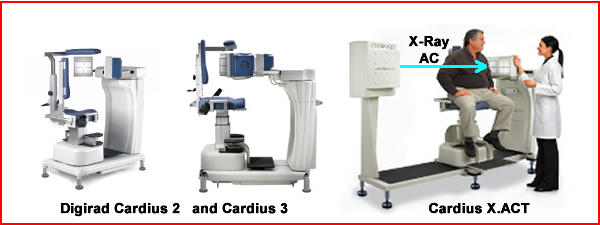
- A third concept looks at the totally digital imaging system. While we will discuss this in more detail later this semester let us bring up the basic topic for discussion
- One, two, or three 3 heads are available. How does impact our acquisition time?
- The Cardius X.ACT generates low energy X-rays that is used for attenuation correction
- Patient positioning is completely different, where the patient is imaged upright not supine
- The patient rotates around the detector while the detector(s) remain stationary

- There is also a triple headed system that has been used in the imaging of the myocardium. But the question is what is best acquisition parameters for acquiring the LV? Single, dual at 180 degrees, dual at 90 degrees, or triple with each head scanning 120 degrees around the circle?
- The overall argument is that the dual headed/90 degree angle is the best where only 180 degrees data is acquired around the circle. Simply it is the best and most time efficient way to acquire cardiac data. However ...
- An argument can be made for 360 degree acquisition, whoever, doing so a triple headed system would be the preferred camera
- Comparing the two acquisition formats
- If you are a 180 fan ...
- The more appropriate counts are found in the left anterior and left side of the chest cavity
- Attenuation of spine, ribs, and opposing lung gives give poor photon data if the other 180 degrees were acquired (This assessment might differ if attenuation correction was available)
- Cannot apply (mathematical attenuation coefficient because of the many different types of densities, which would be significantly affect image quality, if right side of the body was included
- If you are a 360 fan ...
- The only thing 180 is good for is to reduce your acquisition time
- Greater degree of artifacts are generated with 180 because of the loss of counts from the "back side of the heart"
- Posterior/ inferior wall counts are lost and is relates to from poor counting statistics
- Reconstruction algorithms are based on 360 format not 180
QC Procedures
- Center of Rotation (COR)
- Should be done weekly
- Variation should be < 0.5 pixel (but this may vary within different manufacturers)
- If the detector is out of alignment, the images acquired will not truly not represent the same 3D space. Can cause artifacts and/or false data (future lecture)
- COR should be checked on a weekly basis
- Uniformity Correction Matrix
- Should be completed monthly
- 30M for 64 matrix
- 120M for 128 matrix
- Protocols will vary based on
- Type of radiopharmaceutical being used
- Type of collimator being used
- Daily Uniformity Flood should be done to assure uniformity of all the PMTs
- When acquiring SPECT defects will be generated if there is a change in in PMT counts (increased/decreased counts) which will be amplified when acquiring 32/64 projections.
-
57Co flood will assess in daily uniformity analysis, however, when collecting the correction matrix it is suggested that 201Tl or 99mTc aviatrixes be used pending the radionuclides used in your department
Patient Positioning (Application for all radiopharmaceuticals)
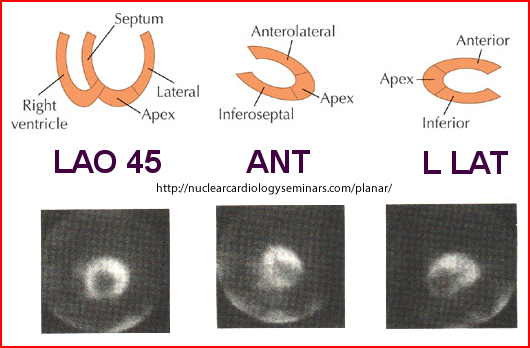
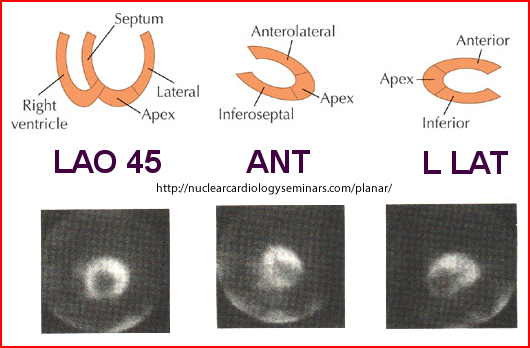
- Planar Imaging - while planar imaging is rarely done a quick review is appropriate
- Usually three views are acquired
- Anterior
- LAO 45 degrees
- Steep LAO 75 or > degrees or L-Lateral
- Position
- Supine for ANT and LAO
- Detector may have a slight caudal tilt
- Steep LAO or L-LAT: patient should be in the lateral decubitus position which will reduce diaphragmatic attenuation and LV inferior wall artifact
- Comments on image quality related to positioning
- Always repeat the exact same angles for Stress and Rest
- At the LAO 45 the vertical long axis is obtained and should resemble an ellipse
- ANT shows the horizontal angle
- Steep LAO gives the best image of the septal wall
- Two minutes images will confirm correct positioning
- On the LAO image if a "donut" shape LV is not see adjust it
- Heart orientation varies from patient to patient
- SPECT imaging overall comments
- Patient should be in the supine position
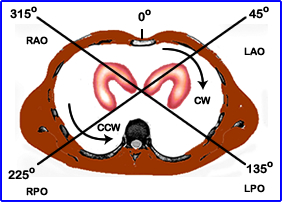
- 180o acquisition starts at the 45-degree RAO and goes to a 135-degree LPO
- Comments on image quality
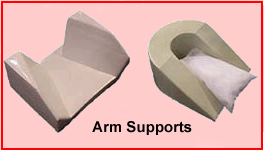
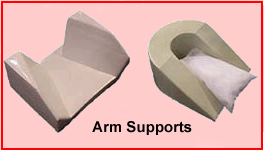
- Patient's arm should be moved out of the field of view. Devices at the head of the imaging table can be used to assist the patient in keeping his/her arm(s) above the patient's head
- Keep the detector head as close as possible to the patient
- Use body contouring
- If contouring is not available then image in an elliptical orbit, do not use circular
- Prevent patient motion (if possible) because motion causes misalignment of the LV
- Prevention includes: explaining this to the patient prior to imaging, watching the patient when imaging, and not distracting the patient during imaging
- There is motion correction software available and it does have some success
- While a point source can be employed to note patient movement this really isn't necessary. Simply review the raw data in cine mode to determine if the LV "jumps" as it rotates around its axis
- If motion continues to be problem, then planar imaging should be considered
- Video on Motion Correction
Planar Acquisition
- Using 201Tl
- Stress
- After the patient reaches the appropriate stress level imaging should be started ASAP
- Acquire 10 minutes per view
- Views: ANT, 45-degree LAO, and Steep LAO acquire
- Collimation: GAP or HR
- 64 or 128 matrix
- Redistribution (Rest)
- Start at 3 -5 hours post stress
- Repeat imaging parameters as seen above
- Keep the imaging angles exactly the same
- Imaging can be done up to 24 hour post injection to evaluate myocardial viability, however, this step can be avoided if 0.5 to 1.0 mCi of 201Tl is injected 15 minutes prior to acquiring the redistribution images
- Planar imaging can also be done with the 99mTc cardiac agents
- SPECT is recommended over planar
- The only situations where planar might be done is to: improved patient cooperation, COR failure, or mechanical problems
- Setup up acquisition as thallium: matrix size, acquisition time, collimation
- Acquisition times should be followed just like the 1-day and 2-days protocols are done below
- Gating is recommended with this procedure
SPECT
- Matrix
- Matrix 64 x 64 use either 32 or 64
stops
- Recommend 32 stops at 40 seconds per stop with 201Tl
- Recommend 64 stops at 20 seconds (or longer per stop) per stop with 99mTc
- 64 stops at 128 matrix at 20 seconds per stop can be employed with 99mTc agent - What might the disadvantage be if this protocol was employed?
- Stops and times vary based on the amount of detectors and the type of radionuclide used
- Upward creep can be an issue whenever acquisition is started less than 15 minutes after the stress test - the key is to make sure that the heart has returned to its resting state
- When a patient achieves a high level of stress the heart moves downward into the thoracic cavity. Associated with high tidal volume the diaphragm and the heart moves downward
- After the stress test, the heart and diaphragm slowly move upward causing "upward creep"
- Usually upward creep occurs in thallium imaging because imaging may start within 5 minutes post exercise. The rational to start imaging ASAP
- Gives you a more accurate heart to lung ratio. High levels of background are associated with CAD
- The longer you wait post 201Tl injection the greater the chance for "minor" redistribution to occur
- Starting acquisition immediately may result in "catching" excesses upward cardiac movement, as much or greater than 2 pixels (not a good thing)1
- Defect seen on the tomographic images would be on stress and may include the inferior and/septal inferior wall
- In the end is there really a good answer to this problem? No, but at least you are aware of it
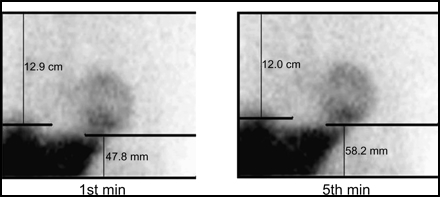
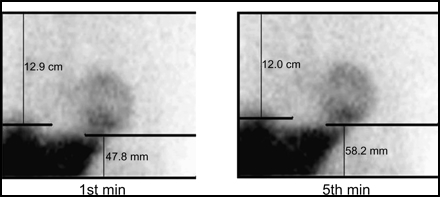
- Lung to heart ratio
- Upper end of normal for 201Tl is 0.37 to 0.55
- Upper end of normal of 99mTc is 0.42 to 0.56
- Above the upper normal limit CAD should be considered
Gating
- Issues to consider when gating the myocardium in the SPECT format
- Thallium vs. 99mTc-cardiac agent
- 8 vs 16 bins
- Gate the Stress (and?) Rest images
- This is discussed in detail in your SPECT Gated lecture
Where do you set the acquisition parameters for normal and dextrocardia patients?
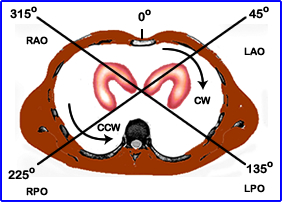
- For Normal patients the heart is positioned on the left of the thoracic cavity (normal)
- Camera should start in the 315o RAO position
- Move CW
- End 180 degrees at the 135o LPO position
- Dextrocardia patients have the myocardium located on the right side of the thoracic activity
- Camera should start at the LAO 45o LAO position
- Move CCW
- End 180 degrees @ 225o RPO position
99mTcSestibmibi/Tetrofosmin Acquisition
- One day protocol
- Resting Acquisition
- Inject IV 10 mCi
- Wait 30 to 60 minutes post dose before imaging. Target to bkg may allow you to image sooner with Tetrofosmin
- If necessary, when excessive activity persists in the hepatobiliary system a fatty meal or cold water may help "wash it out." Questions:
- Where does the activity go?
- Does this affect your imaging quality?
- Imaging may be done either planar or SPECT (SPECT is preferred)
- Gated left ventricle to evaluate wall motion should always be done. Refer to lecture
- Gating can be done with both stress and rest procedures
- However, in most institutions gating is only done in the stress procedure
- As soon as the resting images have been acquired the exercise portion of the test may begin
- Stress Acquisition
- Monitor the patient with a 12-lead EKG
- Exercise the patient to his/her target heart rate [(220 - age) x .85] or greater level
- Inject IV, 30 mCi and continue exercise for one more minute
- If the patient reaches 85% or greater usually the target to background allows imaging to occur within 15 minutes post injection
- If necessary cold water can be given to facilitate hepatic flow
- Usually Tetrofosmin clears faster than Sestamibi, but it has been my experience that cardiac that as soon as the heat reaches its resting state, post treadmill (plus 85% stress), imaging can begin
- Acquisition times vary at different institutions, however the critical issue remains - target to bkg
- Imaging may be done either planar or SPECT (SPECT is preferred)
- Imaging should also include gating the left ventricle to evaluate wall motion
- Image represents myocardial perfusion at the time of exercise
- Contraction represents regional wall motion during rest
- Wall thickening indicates viable myocardial tissue
- Interference of activity rest to stress
- Because there is no change in the energy states 99mTc Stress minus 99mTc Rest doesn't work
- While protocols have been developed where exercise can be done first, this approach is not recommended. Why?
- If there is too much activity in the left ventricle following the rest study, this may mask a defect in the exercise study
- Calculating the stress to rest ratio
- Example: 10 mCi is administered at rest and two hours later 30 mCi is administered for exercise. What is the ratio?
- 10 mCi x .795 (df) = 7.94 mCi
- 30 mCi/7.94 mCi = 4.0 ratio
- What is a good Cardiac stress to rest ratio?
- Cardiac dose based on Image Wisely
- Two day protocol
- Stress followed by rest is preferred, but either procedure may be done first
- Suggested if the patient is bariatric
- Procedure
- For each procedure 20 - 30 mCi can be administered
- In most departments the preferred 2-day protocol usually occurs with bariatric patients. Why
- All other protocol is the same as the one-day protocol
- Advantage
- Better image contrast and improved ability to detect reversible defects
- While image quality is improved, the diagnostic ability seems to be the same (1 vs. 2 day)
- Disadvantage - Will the patient show up the second day of his/her test?
Dual isotope option - While this procedure is not usually done in the Richmond area, it is a popular in other parts of the country
- Setup
- Resting is done first
- Inject IV 3 - 4 mCi of 201Tl
- Wait at least 15 minutes before starting the acquisition
- Collimator LEHR or GAP
- SPECT acquisition - See Thallium Protocol
- Once the acquisition has been completed you may continue with the stress portion of the exam
- Stress Test
- Setup the patient with a 12 lead EKG
- Stress patient with treadmill or pharmacological agent
- Inject patient at peak exercise with 30 mCi of 99mTc-agent given IV
- Continue stressing for 1 more minute
- Image as soon as target to Bkg is appropriate
- Acquisition
- Collimation use LEHR
- Suggest 64 x 64 matrix
- 25 to 40 seconds per stop for 32/64 stops
- What is the rational for doing this procedure?
- The exam takes less time when compared to other MPI procedures. Estimated time of completion is 2 hours
- In the end the main reason to do this procedure is to increases patient through put
- Good new is that this procedure has been show to produce accurate reliable data
- Issues to considered
- Resolution of the thallium is considered suboptimal when compared to the 99mTc agents
- When using quantification portion (QPS/QGS) make sure that you select the correct standards
- You can take delayed images with 201Tl, up to 24 hours post dose, to determine if there is viable myocardial tissue
- The problem you will run into is that there maybe some cross-talk from 99mTc-agent
- 201Tl should is suggested for myocardial viability procedure
- Setup is just like the stress procedure except that you do not stress the patient
- Following injection, 15 minutes post dose, SPECT images can be acquired
- Wait 3 - 5 hours and re-image using the same imaging protocol
- You can also image up to 24 hours post injection
- Issue
- At very high levels of coronary stenosis thallium will take a long time to redistribute
- Therefore, the initial resting imaging may be looked at as "stress" portion of the exam where a myocardial wall lacks activity
- The delayed images then become the redistribution portion of the exam
- If there is/are any reversible defect(s) then viable tissue is indicated making the patient a candidate for re-vascularization
Use of Positrons Radiopharmaceuticals - See lecture
General comments on the use of PET radiopharmaceuticals in myocardial perfusion imaging
- 82Rb is the most commonly used PET agent at this time
- It is considered a perfusion agent
- Has a 75 second half-life
- Uses a generator who's parent is 82Sr
- Rest/stress procedure using vasodilation
- Points of interest
- Generator build up of 82Rb
- Look at the time it takes to complete a stress/rest procedure
- Advantage of a 511 keV vs 140 keV
- Spatial resolution
- 82Sr/85Sr breakthrough
- Compare 18F to 82Rb
- 18FDG used as a viability agent
- It appears that FDG is slightly better than 201Tl in a study of 23 pateints4
- According to the literature when ischemia reaches >90 stenosis the tissue becomes anaerobic, which causes an increase need for glucose
- Comparing gated 99mTc to FDG 23 patients and 361 segments were evaluated. FDG found 30% more viable segments when compared to 99mTc and 99mTc found one viable segment that PET had missed.4
- When comparing MRI to PET to 201T several conclusion could be identified with this population 116 patients5
- 201Tl did correlate well
- MRI detected more smaller infarcts
- FDG found more viability
- MRI did a better job when compared to SPECT in relationship to defining artifacts and infarcts
- Other reason to use PET myocardial imaging
- Bariatric - 511 keV vs 140 keV
- Resolution is better with PET
- 82Rb vs 99mTc-sestamibi in a large population showed sensitivity 90% to 85% and specificity 88% to 85% respectively6
- 99mTc tracer compared to18
F-flurpiridaz
- article

- The future of PET cardiac may be a drug that is in Phase III trails Flurpiridaz. You can see the difference in its ability to find disease
Return to the beginning of the document
Tl-201 Procedure
99mTcSestamibi Procedure
Procedure guidelines from SNMMI on MPI
Return to the Table of Content
1 - "Upward Creep" of the Heart: A Frequent Source of False-Positive Reversible Defects During Thallium-201 Stress-Redistribution SPECT. Friedman, et al m(1989) JSNM
2 - Comparison of Same-Day Protocols Using
Technetium-99m-Sestamibi Myocardial Imaging by
Heo, J. et al.
3 - Suggested reading about the different MPI agents (some are no longer used) - Myocardial Perfusion Imaging Protocols: Is there an Ideal Protocol? by Husain, SS
4 - Comparison of 18FDG PET with thallium SPECT in the assessment of myocardial viability. A segmental model analysis by Alexanderson E, et al. (2006)
5 - 18F-FDG PET for Detecting Myocardial Viability: Validation of 3D Data Acquisition by Brogsitter, C, et al. (2005)
6 - Myocardial viability by contrast-enhanced cardiovascular magnetic resonance in patients with coronary artery disease: comparison with gated single-photon emission tomography and FDG position emission tomography by Wu YW, et al. (2007)
6 - Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease?: A systematic review and meta-analysis by McArdle, et al. (2012)
2/23