Imaging with MIBG
- Anatomy and Physiology
- Pheochromocytoma is a neuroectodermal vascular tumor of the chromaffin tissue usually found in the adrenal medulla, however it can be found ectopically
- Development
- Excess chromaffin tissue is found in children (considered normal)
- At the age of 3, these sites usually regress and are usually found in the adrenal gland
- Extra-adrenal sites include the sympathetic ganglia and carotid bodies (abnormal)
- Other sites can form any between the base of the skull to the bladder (abnormal)
- Usually occurs in the adult population (90%), put can also found in children
- Physiology
- Tumors produce catecholamines which are epinephrine and norepinephrine
- Epinephrine secreting tumors are usually found in the adrenal gland
- Norepinephrine maybe secreted by tumors in the adrenal gland or at extra-adrenal tumor sites
- Characteristics of this hyper-secretion (norepinephrine and epinephrine) cause intermittent hypertension
- Tumor are usually non malignant and can also be found in children
- Indication of tumor includes catecholamine metabolites found in urine
- Neuroblastoma are malignant tumors
- Primary occurs from the adrenal gland or sympathetic nervous system specifically ganglia located in the abdomen (~67%)
- Primary tumor may also arise form chest, neck, pelvis, or spinal cord (~33%)
- Usually occurs in the pediatric population below the age of 10, with over 1/2 occurring before the age of 2
- In the US there are approximately 650 cases per year
- Diagnosing the disease
- Imaging the disease in with nuclear medicine or CT is usually for the purpose of location not for diagnosis
- CT is usually the method for finding the disease. However, when CT is equivocal or when there is a concern of tumors located outside the adrenals then the use of MIBG becomes necessary
- Note – tumor can be found between the bladder and the base of the skull
- Imaging with MIBG
- MIBG is iobenguane or meta-iodobenzylguanidine
- It can be tagged to 131I or 123I
- Contraindicating for this procedure includes: cocaine, Ca-blockers, decongestants, anti-psychotics, catecholamine, reserpine, and a list all drug interactions
- Lugol's solution should be administrated daily, one day prior and up to one week post injection to block the thyroid
- Dose
- 131I 500 to 1000 μCi or
- 123I - 3 to 10 mCi of 123I-MIBG
- Pediatric dose will be less, however, the minimum recommended does is 0.135 mCi of 131I-MIBG
- Pediatric dose for 123I-MIBG suggest 0.14 mCi/kg
- Imaging with of 131I-MIBG
- Planar or whole body to include head to mid-thigh
- Scan speed should be as low as 6 cm/minute and static images should be at least 15 minutes per view
- images can be done at 24, 48, and 72 hours
- Imaging with 123I-MIBG
- Same views as above
- Scan speed may be increased slightly and well as a reduction in time for static images
- Six and 24 hour images should be taken
- SPECT may also be considered - 64 matrix, 360 degrees, sample every 3 to 6 degrees, and 30 to 45 second per stop (literature does not indicate how many head the camera has)
- In addition, renal imaging with DTPA is recommended for localization of the kidneys (where are the adrenal glands located?)
| Organ | 131I - rad/ dose | 123I - rad/mCi dose |
| Adrenal | 0.8 | 0.059 |
| Kidneys | 0.3 | 0.048 |
| Urinary Bladder Wall | 2.8 | 0.311 |
| Pancreas | 0.4 | 0.056 |
Normal findings
- Faint visualization of adrenal medulla and occurs in 16% of studies
- Maximum liver uptake occurs within 24 hours
- Urine excretion is seen in 60% cases of patient for up to 24 hours
- Large bowel uptake is noted in 20% of patients
- Salivary glands will visualize
- Higher concentrations of activity is seen in the heart (why?)
Abnormal
- Abnormal uptake in the adrenal medulla
- Uptake outside the adrenal glands is defined as extra-adrenal sites
- Tumors in the bladder can be missed and is do to normal bladder activity
- Sensitivity for pheochromocytomas is between 85 to 90 percent
Example
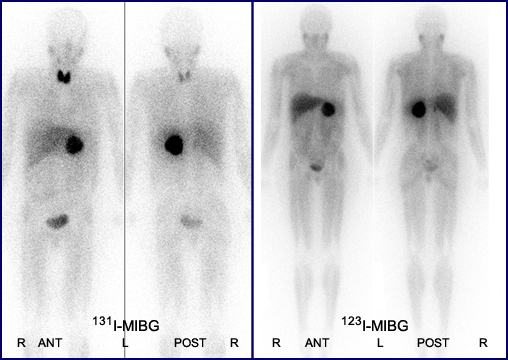
- Compare the two MIBG exams and note that it is exam of using both iodines. Can you appreciate the difference? Is one better than the other?
- In 131I-MIBG the patient has a Pheochromocytoma in the left adrenal. http://en.wikipedia.org/wiki/Iobenguane
- 123I-MIBG is a different patient that also has a pheochromocytoma located in the left adrenal. http://gamma.wustl.edu/newtfh/general/combined/submitted_130879.html
- Should you see thyroid uptake? What does this anomaly indicate?
Application of therapy
- 131I-MIBG if given in a large enough dose case be used to treat paragangliomas and pheochromocytomas.
- Candidate for treatment
- Children older than 12 years of age
- Tumors that cannot be surgically removed
- Spreading to other parts of the body
- Clinical study completed by Pryma, DA, et al. treated neuroendocrine tumors
- ~500 mCi per dose (18.5 GBq) given IV
- Of 68 patients approximately 92% has a partial response and stabilized the disease within 12 months
- Adverse reaction were nausea, myelosuppression, and fatigue
- There was no hyperactive response to the medication
- Candidate for treatment
Return to the beginning of the document
Return to the Table of Contents
Continue to the Power Point Presentation
Reference
Efficacy and Safety of High-Specific-Activity I-131 MIBG Therapy in Patients with Advanced Pheochromocytoma or Paraganglioma by Pyrma, DA, et al., JNM 2018