- 99mTcPyrophosphate (PYP)
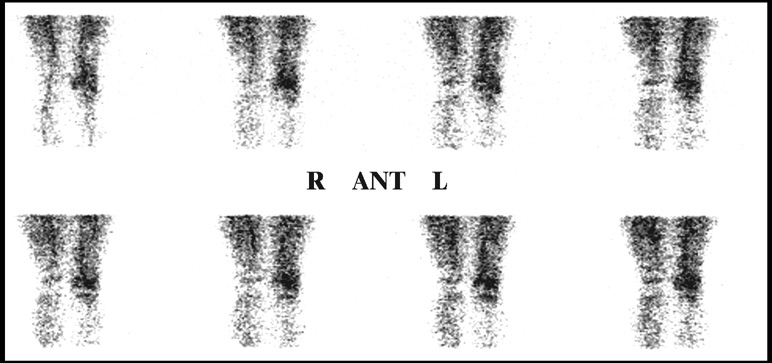
- This agent is really not used as a bone agent because MDP has improved target to background when compared to PYP
- PYP is mostly used for cardiac imaging because of its high Tin (Sn) level. Sn reduces 99mTcO4- allowing pertechnetate to tag to the RBC thus allowing the ability to image the vascular pool (GI bleeds and gated cardiacs)
- 99mTc Methylene diphosphonate (9mTcMDP) is the agent most routinely used agent to image the skeletal system
- It has greater target to background
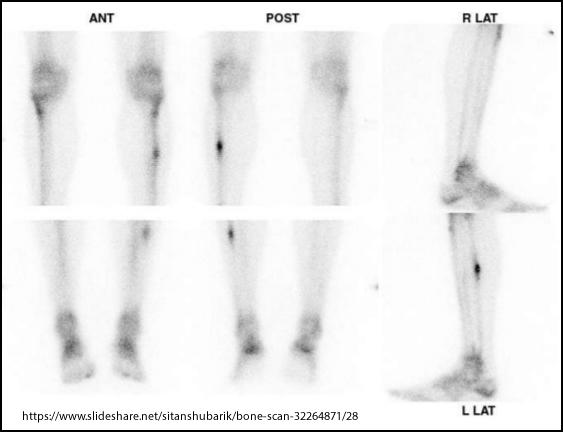
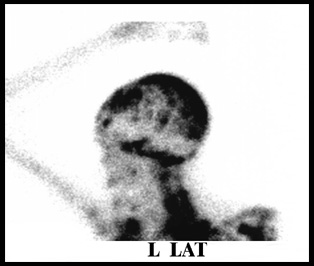
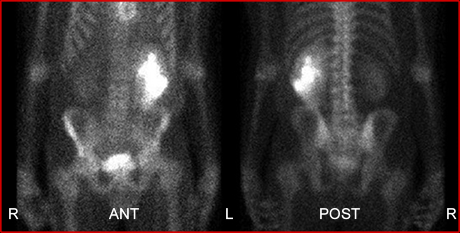
- Consider target to background in the above images. What comments might you have?
- Why do you think there is such a difference between the two?
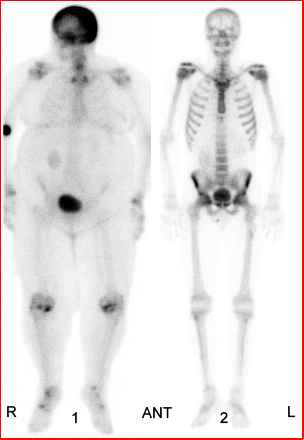
1 - http://www.med.harvard.edu/JPNM/InterestingImages/Case18ii/Dx18.html
2 - http://www.brighamandwomens.org/departments_and_services/radiology/services/nuclearmedicine/patient/bone.aspx
- Must consider vascularity and bone production/turnover
- Uptake is based on radiotracer exchange with ions in the bony matrix known as heterionic exchange. This is also referred to as chemisorption
- Calcium is located on the hydroxyapatite crystal (bony matrix)
- Phosphate compounds exchange with Ca on the hydroxyapatite crystal
- Osteoclasts and osteoblasts work on the bony matrix
- Uptake of the radiotracers increases when there is high metabolic activity
- Usually this activity, in adults, is due to excessive bone destruction (bone turnover) - blastic vs lytic
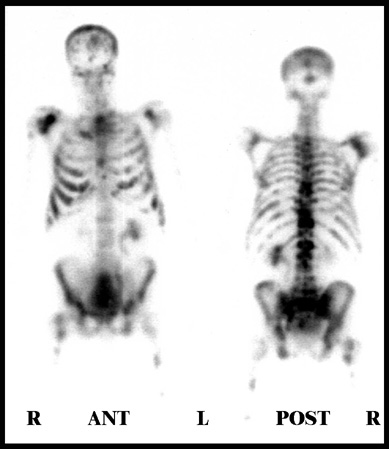
- Normal distribution of radiopharmaceutical
- Up to 50 percent of the injected bone agent will be eliminated through the kidneys within 3 hours
- Fifty to 60 percent of the radiotracer will localize in bone
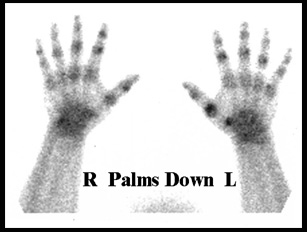
- Concentration of the radiotracer is greater in the central skeleton and less in the peripheral bone (chest vs. hands/feet)
- Consider vascular flow and relate this to tracer distribution
- Consider imaging central skeleton vs. peripheral bone and how it might affect acquisition? Where would the count rate be greater?
- Detector size
- Increasing the size of the detector means increasing its field of view (FOV). In turn, the larger the FOV the greater amount of counts are needed to get the same resolution
- As an example, a 15-inch detector may require a 500k image of the chest, however, a 21 inch detector would require a 1,000k image in order to achieve the same count density
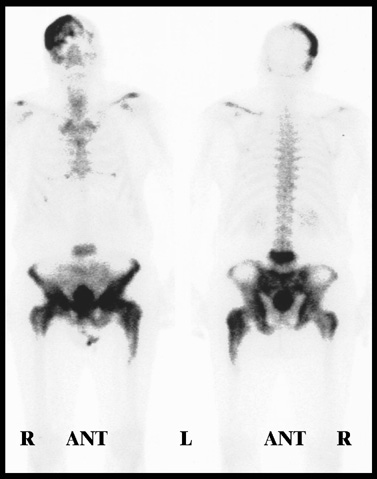
- Bladder activity may obscure lesions located within the pelvis - remember 50% is excreted out the kidneys
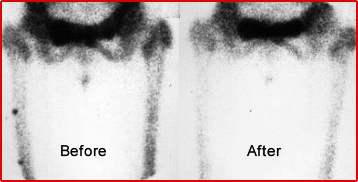
- Urine on the clothing or skin may create a lesion artifact within the bone and/or soft tissue hot spots were discovered in the above scan. The patient was asked to wash her leg then re-imaged. Has the image changed?
- Hydration improves the quality of the scan by increasing urine production and therefore eliminating more radiotracer from the soft tissue. This improves target to background
- The body is bilaterally symmetrical; hence, asymmetry in a bone scan may indicate disease
- If urinary tract obstruction is suspected, ambulate the patient, have the patient void, and re-image. This patient has a recto-sigmoid tumor pressing against the left ureter
- 99mTc to is very sensitive to O2. It breaks down the Tc - MDP tag
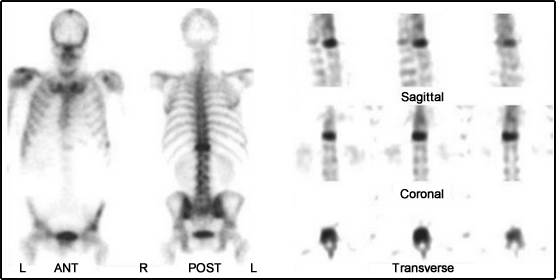
- Images are taken in several different formats
- Dynamic (flow) study
- Immediate and delayed static images (delays usually occur 2-3 hours post-injection)
- Whole body or static images are taken on delays
- Single Emission Computerized Tomography (SPECT) will be discussed later
http://www.slideshare.net/lahollenbeck/the-bone-scan
http://www.wjnm.org/article.asp?issn=1450-1147;year=2014;volume=13;issue=2;spage=132;epage=134;aulast=Marzooq
Types of Bone Scans
- Dynamic (flow)
- Pooling (early or immediate)
- Delays (3 hours)

- Requires a large field of view camera
- The detector will image the entire body (top of head to the end of the feet)
- Usually acquire a scan speed around 12 cm/minutes (or less).
- This indicates the speed in which the table or detector moves across the patient
- Slower speeds will give greater counts and will improve count density
- Most systems have dual heads which is more efficient than a single head because you acquire both anterior and posterior images at the same time
- Whole body contouring further improves resolution
- Increasing distance (patient to detector) significantly reduces resolution and increases scatter counts
- Don't forget the urinary bladder. Too much activity in that area will cause a loss of bone detail. This is a concern, especially if there is disease in the pelvic region. Have the patient empty his/her bladder before re-acquiring the data
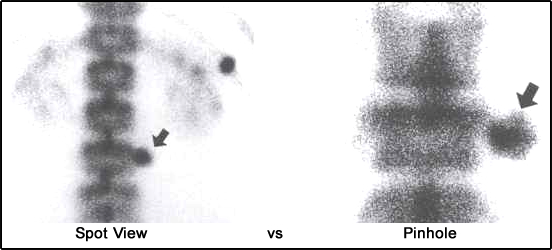
- Most bone scans image the entire body, however, sometimes a limited bone scan is ordered. This requires data to be collected only in a specific area within the skeletal system
- Feet, hands, wrists and elbows are examples of when a spot view might be ordered
- A limited bone scan may or may not include a three-phase bone scan
https://www.mussenhealth.us/intense-tracer/introduction-and-fundamentals-of-pinhole-scintigraphy.html
- Pinhole collimator may be used to magnify specific areas of interest (head of the femur, patella, and/or bones in the feet or hands
- In order to acquire this high resolution image, remember that the acquisition will take a long time - Why?
- Consider the inverse relationship between resolution and sensitivity
- Remember an image must have enough counts to resolve the magnified area of interest
https://www.slideshare.net/sitanshubarik/bone-scan-32264871/28
- Should be used when bone disease involves overlapping bone (ex. spine or mandible)
- A whole body bone scan may look normal in the spine and show a hot spot within a vertebral body when SPECT is used