- Planar is 83% sensitive and 88% specific
- Combination of the literature indicated a mean sensitivity of 86% and a mean specificity of 85%
- 79% sensitivity with patients that did not have a prior infarct
- 96% sensitivity with patient that have had a previous infarct
- Looking at C and D, what does that tell you?
- Planar imaging 90 and 70% respectively
- Quantitative and planar imaging: 90% sensitive and 75 to 80% specific
- SPECT quantitative results show: 87% sensitivity and 79% specificity
- Other literature has shown a high correlation between 201Tl and 99mTc
| Exercise | Adenosine | Dipyridamole | Dobutamine | |
| Sensitivity | 84 | 88 | 87 | 91 |
| Specificity | 87 | 85 | 81 | 84 |
- Approximately 35 to 40 percent of MPIs are done pharmacologically
- Dipyridamole SPECT shows 97% sensitivity and 93% specificity
Treadmill Dip-Echo Dob-Echo DIP-MIBI Dob-MIBI Sensitivity 58 55 61 97 91 Specificity 67 96 96 89 81 Accuracy 62 73 77 93 87
- Treadmill is EKG stress (no imaging)
- Dip = dipyridamole
- Dob = dobutamine
- Echo = Echocardiography
- MIBI = sestamibi
- Imaging quality - PET excellent 78 and 79% vs SPECT excellent 62 and 62%
- Gating - PET excellent 96% and SPECT 81%
- Accuracy for stenosis @ 70% - PET 89% and SPECT was 79%
- Accuracy for stenosis @ 50% - PET 87% and SPECT 71%
- PET has improved accuracy in both men and women that were and were not obese
- PET has improved detection with multi-vessel disease (MBF/R)
- May increase sensitivity and reduce specificity. Why does this happen?
- All your positives are sent to cardiac cath and a certain percentage of these are going to be false positive.
- False positive data is used to calculate your specificity
- Few if any of your negative exams are sent to cardiac cath which generates bias in your sample falsely elevating your sensitivity
- The only way to truly determine sensitivity and specificity is to get a true random sample of your population
- Bayes theorem is another issue that indirectly relates to this and is discussed below
- Single vessel disease = 79%
- Double vessel disease = 88%
- Triple vessel disease = 92%
- Sensitivity appears to increase slightly while specificity seems to decrease slightly
- This may be caused by referral bias
- One study showed that SPECT was superior
- In male patients
- Milder disease with no previous infarct
- Single vessel disease where the artery was 50-69% stenotic
- Two questions must first be considered
- What is the probability of the patient having disease if the results are positive?
- What is the probability of the patient not having disease if the results are negative?
- Initially determine the pre-test likelihood of disease - setup parameters
- Asymptomatic
- Chest pain = sub-sternal location, provocation by exercise, and pain relief via nitroglycerin
- Typical angina = all the
- Atypical angina = two of three
- Non-angina = one of three
- Pretest likelihood of disease affects the post-test likelihood of disease
- In an asymptomatic patient, pretest probability of having diseases is 5%. The results then indicate only 20% that have a positive stress test are truly positive, while less than 1% of the negatives are false negative
- In classifying those patients with an intermediate likelihood of CAD the pretest probability is 50%. [post test] Of those patients that have a positive test, 90% will be true positives, while those that are negative have less than 10% of being false negative
- High pretest likelihood (typical angina) of CAD has a 90% likelihood of disease. [post test] Of those that are positive 99% are true positive, while of those that have a negative scan, 75% are false negative
- Conclusion:
- Does a nuclear cardiology exam benefit patients with low probability of disease?
- When should nuclear cardiology be ordered on a patient?
- Of the classifications above, which group of patients receives the most benefit when Bayes' theorem is applied?
- What is the value of taking a patient's history?
- A little more information on sensitivity/specificity/accuracy
- True-positive = sensitivity
- True-negative = specificity
- Sensitivity + specificity = accuracy
- LAD, LCX, RCA
- Sensitives are 69%, 37%, and 65% respectively
- Specific 94%, 95%, and 85% respectively
- Comments on why 201Tl has low sensitivity
- In patients with multi-vessel disease
- More than one area will be ischemic, however, only the more hypo-perfused area is identified. Inability to identify all the regions may relate to the variations of count density and the contrast between the different regions of perfusion
- The stress test may be terminated at sub-max due to ischemic developments. The area that caused the ischemic event will be identified; however, if other area(s) exist that would cause ischemia, but is/are not as stenotic as the one that caused termination of the stress test, then blood flow to the less stenotic areas may appear normal. Hence, the importance of achieving maximum heart rate is essential in order to define all ischemic areas
- 50% or less narrowing of a coronary does not lead to ischemia or hypo perfusion, but can be seen in angiography
- Collateral circulation may prevent an area from becoming ischemic
- Quantification of planar imaging has improved sensitivity and specificity
- SPECT and its role with detecting CAD
- LAD - 75% and 85% respectively
- LCX - 54% and 97% respectively
- RCA - 88% and 84% respectively
- Look at the polar map and consider the anatomy of the LV with its relationship to acquired data and detecting CAD
- Quantification seems to improve sensitivity, but not specificity
- Overall SPECT improves sensitivity, which may be due to improved contrast defining the defect via decreasing the overlapping of the myocardial walls (when compared with planar)
- Multi-vessel disease
- When all three vessels contain disease, hypo perfusion to the entire LV may show uniform uptake, and indicate a false negative study
- Quantitative analysis may improve the detection rate of multi-vessel disease (looks at the washout curves)
- One aspect to note with visual analysis is to determine if the walls to the are LV are very thin - in wall motion, is there thickening?
- Pulmonary uptake of 201Tl
- Increased pulmonary uptake can be related to left ventricular dysfunction or multi-vessel disease
- Draw ROIs around the lung activity at stress and redistribution
- Compare (ratio) to determine the extent of the washout rate from the pulmonary system
- Slow washout may also be due to: mitral valve regurgitation, mitral stenosis, decreased left ventricular compliance, and non-ischemic cardiomyopathy with left ventricular dysfunction
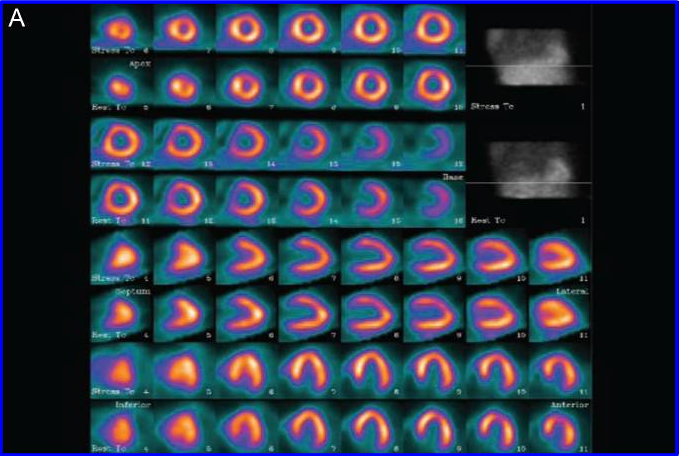
- Example of 3 Vessel Disease with 201Tl - abnormal EKG but normal MPI
- Transient Ischemic Dilation of the LV (TID)
- Multi-vessel or critical stenosis of two or more coronary arteries causes LV transient dilation
- Ratio of stress to rest image (negative for ischemia) is 1.02 +/- ).05
- Ratio of stress to rest images (two vessel disease) is 1.12 +/- .08
- Ratio for stress and rest images (three vessel disease) is 1.17 +/- .09
- What happens to TID as an increase to diseased vessels occur?
- There is also an association with 99mT myocardial imaging agents?
- Transient Ischemic Dilation presenation - Link here
- Studies have shown that 3-4 hour redistribution images that seem as non-reversible may become reversible in 18 to 24 hours.
- One study showed segmental reversibility improved following by-pass and angioplasty
- Another study analyzed late reversibility and identified segments that were considered non-reversible. It concluded that at least 1 segment in 53% of the patients had late reversibility
- Cause may be due to glucose loading OR
- Low regional myocardial blood flow in areas that have severe stenosis
- An interesting article evaluates PET, gated SPECT, MUGA, and echocardiology. It concludes that all modalities work very well in identifying myocardial viability with patients that have CAD. In addition, it appears that MUGA may be the best alternative - 3