- Hyperthyroidism results from excess levels of T3 and T4 which can be cause by several factors
- Classically, the patient is extremely nervous, fatigued, may show weight loss, proximal muscle wasting, eye protrusion, intolerance to heat, and pretibial myxedema
- Nodular goiter
- Signs of hyperthyroidism
- Autonomously functioning cells in thyroid develop and produce excessive amounts of thyroid hormones
- In addition, increased levels of TSH may further exacerbate this situation
- Heterogeneity (no longer homogeneous cell structure) and replication occurs, which form thyroid nodules over time
- These nodules contain hyper-functioning tissue
- In addition, these nodules continue to replicate, resulting in "cloned" nodule
- The term autonomous is important since it indicates that these nodes can still excrete excessive amounts of thyroid hormones, even when the body responds by reducing TSH levels
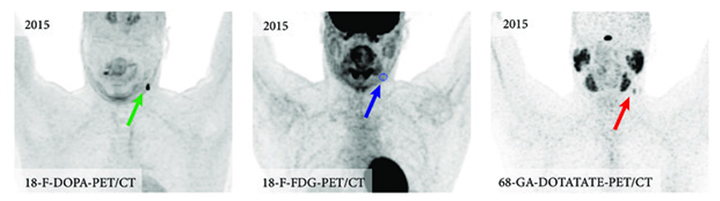
- Over time, hot and cold nodules can be noted in this disease
- Cold nodules may be the response to lower TSH levels, while hot nodules would be considered autonomous in nature
- Also, hemorrhage and necrosis of a hot nodule will result in a cold nodule
- Symptoms: diffused enlarged gland (goiter), hyper-metabolism, exophthalmus (eyes).
- Long Acting Thyroid Substance (LATS) is noted in blood tests, but the reason for this is unknown
- TSH levels are usually low
- Increase levels of T3 and T4. Blood test usually indicate a high level of T4
- About 50% of patients that have this disorder go into remission if left untreated
- More theory on why this happens
- Patients with Graves' disease also have auto-antibodies that may be synthesized by lymphocytes in the thyroid and stimulate TSH receptor within the thyroid (there are two types)
- The two types of of antibodies are: Thyroid stimulating antibody (TSAb) and anti-TSA
- TSAb stimulates thyroid hormone production just like TSH, which may cause Graves' disease
- Radioiodine therapy causes increased levels of anti-TSAb, which reverses the stimulation effect of Graves' disease
- Causes of Graves' disease may be due to: Yersinia enterocolitica, stress, genetic predisposition, and smoking
- There is also an association with some forms of thyroid cancer. In animal research, chronic TSH stimulation has shown an increased incidence in thyroid cancer
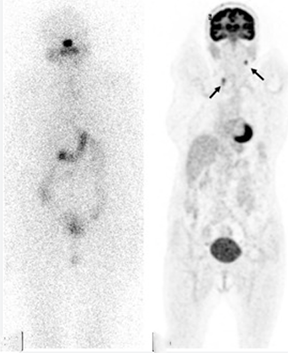
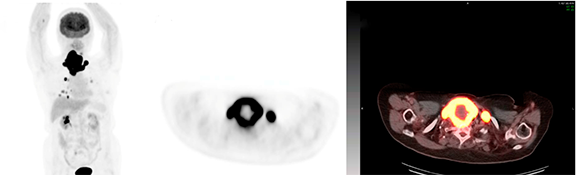
- Usually singular or multiple nodular (rarely) disease. The(se) functioning autonomous nodule(s) pick up excessive amounts of radioiodine
- Causes hyperthyroidism
- The anterior pituitary gland reduces the TSH levels to where there is little to no circulating TSH, however this has no effect in reducing T3/T4 production
- Patient produces increased levels of T3 and T4
- Nodule(s) usually suppress surrounding thyroid tissue
- Administration of TSH will determine if surrounding thyroid tissue is functioning
- See TSH stimulation/suppression test
- 201Tl and 99mTc-sestamibi are alternative radiopharmaceuticals used to see if surrounding thyroid tissue is suppressed
- No circulating LATS
- Usually requires additional 131I for treatment (as compared to Graves' disease)
- May be single, multiple, or autonomous in nature
- Amount and size of nodule(s) will affect the level of hyperthyroidism
- Graves' or Plummer's disease may be associated with toxic nodular goiter
- Abnormal secretion of TSH from the pituitary gland
- May be due to tumor
- Teratomas and a few types of thyroid cancer secrete excess amounts of T3/T4
- This is rare
- It is believed that certain types of viral infections may cause an inflammatory thyroid disorder
- One or more types of viruses may be associated with this process
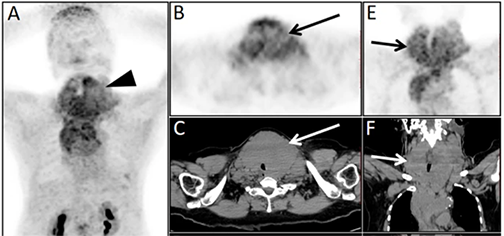
- Usually the entire gland is involved, however, it may start with only part of the gland
- Symptoms will last for 2 weeks to several months
- Initial insult causes a sudden release of thyroid hormones resulting in a hyperthyroid state
- Thyroid uptake and scan usually indicate a hypo-activity which is caused by the initial attack/damage to the thyroid
- Uptake is low
- Impossible to image
- Usually thyroid function returns to normal, however, over several years, the patient may eventually become hypothyroid
- Seems to be an autoimmune event
- Pregnancy affects the immunoregulation
- Usually occurs in the first trimester or at delivery, with the latter being more common
- May recur in succeeding pregnancies
- There are three stages which are not always clinically present:
- Hyperthyroidism
- Hypothyroidism
- Euthyroidism
- May be caused by ingestion of beef products containing bovine rich thyroid hormones
- There may be other known or unknown factors
- It may also be an autoimmune response
- Usually causes transient hyperthyroidism
- Excessive intake of iodine may cause either hypo- or hyperthyroidism
- Refer to the thyroid's biofeedback loop, where the patient becomes hyper/hypo and finally returns to a euthyroid status
- Seen more frequently in places where there is iodine deficiency. In this scenario a patients with limited iodine in his/her diet resulting in an enlarged thyroid caused by increased TSH stimulation (the body is trying to extract limited iodine from the blood pool)
- A sudden response to a hyperactive state occurs when a significant dose of iodine is ingested
- This may also be seen in patient with nodular thyroid disease, where increased levels of iodine cause a hyperthyroid response
![]()
- Patient will appear fatigued, have cramps, and be constipated
- Myocardial contractility is greatly reduced, resulting in a reduction of pulse rate and stroke volume to about half of its normal value
- In severe cases, the patient may be in a comatose state
- Results from an iodine deficient diet; however, this is uncommon in the US
- In addition, thyroid failure can occur via an autoimmune response (note the above autoimmune diseases)
- While most autoimmune and thyroiditis initially start off as a hyper-response, eventually the patient returns to a euthyroid state; however, hypothyroidism may eventually result over time
- The same can be said for hyperthyroid patients being treated with 131I. Treatment usually causes hypothyroidism over time
- Untreated hyperthyroidism (Graves' disease as an example) shows strong indication of the gland eventually becoming hypo-active over time
- Drugs such as lithium and amiodarone may eventually cause the thyroid to become hypoactive
- In general - The inability of the thyroid gland to trap and organify iodine results in lowering iodine uptake, decreased levels of T3/T4, and elevating the levels of TSH and TRH
Explain this effect using the negative biofeedback loop
- This does not occur as often as primary hypothyroidism
- Pituitary insufficiency maybe caused by tumor (adenoma), which results in a decrease of TSH secretion, producing a hypothyroidism
- Poorly functioning hypothalamus will cause reduced secretion of TRH
- Insufficient TRH reduces TSH secretion, which results in a hypo-functioning gland
- This may occur with or without pituitary disease
- Usually results from a T-cell mediated, organ-specific autoimmune response
- Another words, the body attacks its own thyroid
- Continual insult results in fibrotic changes in the gland as well as atrophy of the follicular cells
- Specifically in Hashimoto's disease
- Anti-peroxidase antibodies attack thyroid's ability to organify iodine (peroxidase is responsible for organification)
- Antibodies also inhibit the peroxidase enzyme
- Positive perchlorate discharge test-1 is an indication of Hashimoto's disease
- Clinical symptoms
- Goiter with or without hypothyroidism
- May initially appear hyper-active
- Over time, hypothyroidism results
- Appear lethargic, with potbelly and enlarged tongue
- Physical and mental growth are severely retarded