
Following IV injection of 99mTcMAG3 from the renal artery it enters the afferent arteriole, which goes to the vascular bed of the glomerulus. Here a percentage of the tracer is filtered out by the glomeruli. The remainder of the tracer exits through the efferent arteriole which then travels through the peritubular capillary network. MAG3 is filtered out as it leaves the vascular pool and enters the tubules. From there MAG3 moves through the collecting system to the urinary bladder.
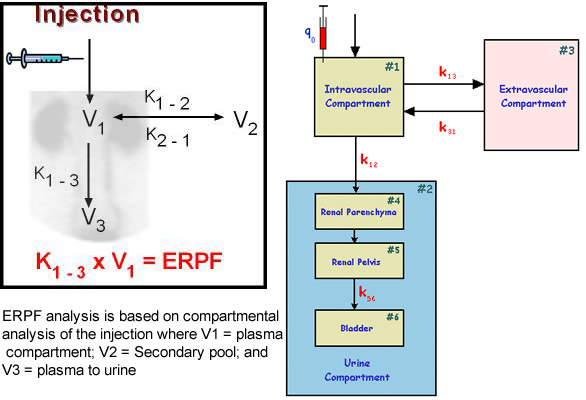
The graph below shows the normal excretion of the radio-tracer with a time activity curve. The diagram on the right explains radiopharmaceutical distribution applying "compartmental pharmacokinetics analysis." Injecting the tracer and its distribution in the body via K1 through K3 with the end result being define EPRF
 |
 |
| The three phases to the time-activity curve relates to renal function and possible disease states, which appear pre-renal, intra-renal, and post renal |
Disease can be pre-renal, intra-renal, or post-renal. General comments are made prior to a specific discussion on specific diseases
Abnormal Renogram
Pre-renal
1. Bilateral function and uptake - poor cardiac output or dehydration causes decreased GFR. Since both kidneys are effected, ROIs will not be able to compare L to R kidney function. Peak (maybe prolonged in both ROIs), and cortical transit (prolonged - both), excretion (reduced - both). Overall, decreased tracer flow through the kidneys is generally noted
2. Unilateral disease may result from renal arterial stenosis (RAS) [This also creates renal hypertension]. This accounts for approximately 5% of all hypertension cases. RAS will show initial uptake but will have a continued prolong cortical transit time. As the disease progresses, the cortical transit will also increase. End-stage renal disease the tracer show no uptake
1. Loss of glomeruli and tubule function result in delayed time to peak, prolonged excretory phase, which will eventually flatten out
2. Tubular Impairment - Initially unaffected, however, over time, tubular excretion reduces, resulting in diminished tracer excretion (increase T1/2). Over time, this will also affect initial tracer uptake to the kidney, causing cortical transit and excretory to be prolonged. At end-stage, the entire renal curve will go flat
3. Intra-Renal Obstruction - The activity curve continues to rise for the entire length of the study because the tracer cannot be excreted. Often bilateral, with post-renal obstruction being unilateral
Post-Renal
1. Obstructive uropathies (hydronephrosis) - blockage caused by stones, tumor, and/or blood clots. Chronic obstruction will result in the loss of renal function
2. Dilated (non-obstructive) ureters is a result of atrophy to this muscular structure - urinary reflux occurs. Use of a diuretic, such as Lasix, will determine if there is an obstruction to a clot/stone/tumor vs. dilated ureters
Disease Specific
Inflammatory disease
Pyelonephritis - Urinary Track Infection (UTI) at the acute stage the kidneys are enlarged with decreased tracer uptake. Chronic UTI results in scarring with significant decreased in tracer perfusion showing minimal parenchymal function. Scarring of the renal parenchyma often occurs with urinary reflux and gets worse over time. Pyelonephritis can lead to hydronephrosis
Abscess - focal area(s) of decreased uptake and avascular in nature. This will also reduce renal function
Use Gallium to evaluate the suspected inflammatory process furtherWhat issue would there be in defining infection with FDG
Obstructive Uropathy - See above
Vascular disease
RAS
Hypertensive disease - See above (Note the use of an ACE inhibitor. This will be discussed later)
Renal Vein Thrombosis - No renal blood flow. Lacks tracer accumulation. Collateral circulation may preserve the kidney
Infarction Can be embolic or atherosclerotic in nature. Decreased uptake and lack of function to the affected area. It may include the entire kidney
Renal Insufficiency - Pending etiology use either DMSA or MAG-3, which depends on the nature of the disorder
Renal Trauma - Cause mild contusion (no effect) to infarction
Congenital Anomalies
Agenesis (lack of organ or part) Not able to differentiate between metanephric mass and ureteric bud. Usually little renal activity is noted
Duplication - Can be duplication of the renal pelvis, from the upper pole calyxes, to an extra ureter. Causes reflux, obstruction, or infection
Supernumerary kidneys - There is an extra kidney. It is usually prone to infection
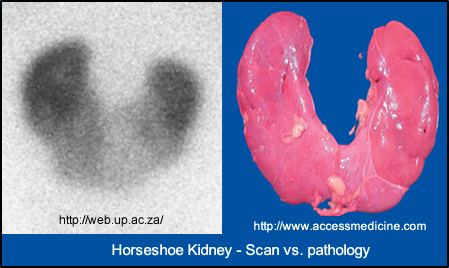
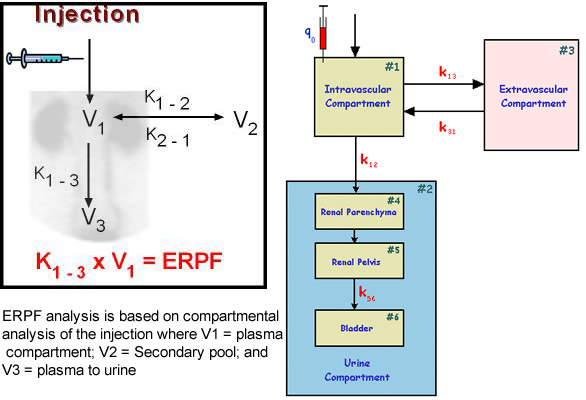
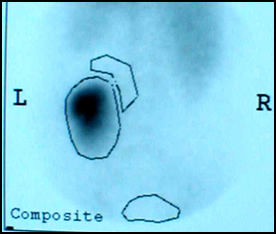
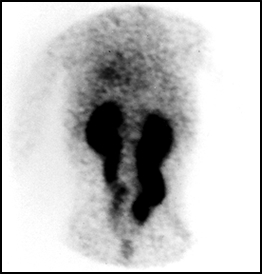
Anomalies of position - Changes in the shape and position of a kidney. The example above of a horseshoe kidney
Renal Transplants
All renal transplants should have a baseline renogram within 24 hrs post-implant. Hence repeating the exam when the patient has complications will help diagnose rejection or other diseases that might occur. Renal Artery or Vein Thrombosis can occur with a renal transplant patient.

Hyperacute rejection - It looks like RAS
Occurs within 1 to 12 hrs post transplantation where antibodies attacks kidney that can be caused by prior graft, multi blood transfusions, or multi pregnancies
Accelerated rejections
This is predominantly cell-mediated and occurs within 1 to 5 days post-transplant. The patient is susceptible to the transplanted kidney
Acute rejection
This is cell-mediated with lymphocytes aggregate to destroy the graph
Chronic rejection
Is an antibody that attacks endothelial and interstitial cells of the transplanted kidney causing: narrowing of vascular blood flow, decreased renal size, hypertension, and ultimately renal failure if the process is not corrected
Acute tubular necrosis (ATN) - Is secondary to ischemia. Renal imaging denotes decreased renal perfusion and increased tracer retention that extends into the excretory phase of the time-activity curve. Usually occurs in patients that are early post transplant. There is a rise in the time-activity curve with no obstruction. Oliguria (decreased urine output) Elevated urinary sodium in noted. ATN is transient and renal function may improve in several days. Proper anti-rejection medication must be given
Acute rejection - Like ATN, however, the time-activity curve becomes progressively worse over time and occurs from several days to weeks post transplant, with fever, hypertension, oliguria. In 80 to 90% of cases, 99m Tc-SC uptake is seen within the kidneys. MAG3 shows decreased function in all aspects of the scan along with a reduced excretion index (EI)
Chronic rejection - Occurs over time. Decreased flow, decreased function. Decreased renal perfusion with radiotracers and normal creatine levels
Obstructive uropathy - Blood clots are seen in the collecting

In this Lasix renogram obstruction is observed in the right kidney via the image and the time activity curve
Complete obstruction of both kidneys with "megaureter." There was no washout of the radiotracer even after 20 minutes post Lasix administration
Hydronephrosis - accumulation of excess water in the calyxes which causes dilation and enlargement. Retention of water is usually do to obstruction
Extravasation

Leakage of urine can occur in the collecting system

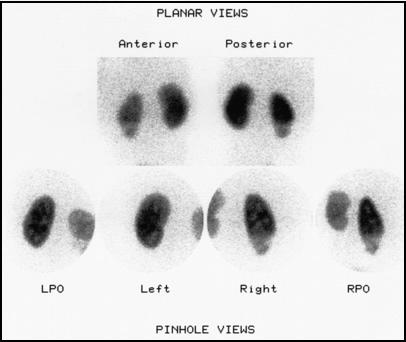
Here are a different types of abnormal kidneys showing not just the nuclear medicine scan, but also what would be seen from an anatomical prospective
Return to the beginning of the page
Return to the Table of Contents
6/23