- This failure results in the reflux of urine from the bladder to the kidney
- There are several degrees of reflux
- Reflux may only occur in the distal portion of the ureter (considered the most mild form of VUR)
- Or reflux may be seen all the way up the ureter and into the renal pelvis (considered the most severe form of VUR)
- Causes of VUR include: congenital, pathological process, infection, or immaturity of the system
- Passive factors of VUR
- Oblique entry of the ureter into the bladder
- Length of the intramural ureter not being long enough
- Length is long enough to not cause reflux
- The tunneling of the ureter indicates that there is a possibility of reflux
- Ureter tunnel is very short and reflux will occur
- If you want to know more about reflux go to http://www.mitrhospital.com/category/vesicoureteral-reflux/19
- Active factors for VUR
- Muscle contraction
- Peristalsis
- Is usually seen in children or infants and as the child grows VUR, may disappear as the length of the ureter increases with age (known as spontaneous cessation)
- Occurs in approximately 1% of the pediatric population
- Chronic VUR causes infection and scarring within the kidneys
- Radiographic voiding cystourethrography (VCUG) [radiology procedure]
- Gives excellent anatomical detail
- Outlines the anatomy of the pelvic calyceal (renal pelvis), ureter, and bladder
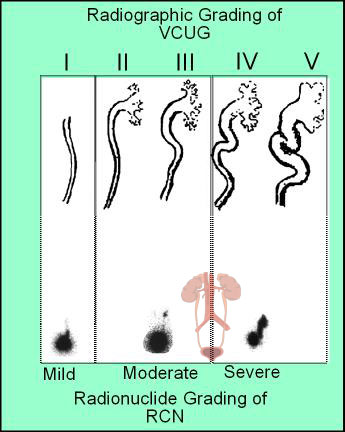
- Shows reflux and severity of the disease (note image below that compare the radiographic procedure with the nuclear medicine procedure)
- Grades I - V
- The higher the grade the worse the reflux
- Disadvantage of VCUG
- High radiation exposure
- Low temporal resolution prevents the diagnosis of intermittent VUR
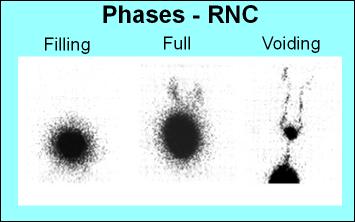
- Radionuclide cystography (RNC)
- Advantages
- Low radiation exposure
- High temporal resolution
- High sensitivity in detecting VUG
- Disadvantage is that it is unable to delineate between the bladder and urethra and its resolution cannot show anatomical detail
- The above images compare the severity of reflux of urine from the urinary bladder, up the urethra, and finally into the renal pelvis
- These images compare VCUG to RNC
- Note the detail seen in VCUG
- While there is lack of detail in the RNC, one is still able to define the severity of disease
- Remember the greater the amount of reflux, the greater the severity of VUR
- There are two types of procedures: direct and indirect
- Indirect RNC is nothing more than a renal scan in which the radiopharmaceutical is administered IV
- Following the administration of 99mTcDTPA, a renal scan can be taken
- Ideally imaging should be started when there is no residual activity in the renal pelvis
- The patient is not allowed to void until activity is no longer seen in the kidneys (obviously this requires complete patient cooperation - consider the possible difficulty if it is a pediatric patient)
- Dynamic images are then taken while the patient is sitting upright and voiding into a bedpan or urinal
- If residual activity is noted in the renal pelvis or urethra, then VUG can be diagnosed
- This is not the preferred method
- Direct RNC
- Patient preparation
- Urethral catheterization is completed with the patient
- Once catheterization has been established, drain all urine from the patient's bladder
- Determine the amount of urine the bladder can hold given the following formula
- Depending on urine volume obtain a 200 to 500 mL bag of saline
- The above formula calculated the approximate size the child's bladder based on age
- Prepare a 1 to 2 mCi of Tc99mDTPA and draw into a syringe
- Place the saline bag on an IV pole and elevate this above the patient
- Connect the saline bag to the catheter
- Patient should be in a supine position, on the imaging table with the camera placed underneath the patient with the detector within the area of interest
- Set the camera up to collect two dynamic images
- 1 to 2 second per frame for 30 to 60 minutes
- One is labeled filling the other dynamic is labeled voiding
- Several static images should also be prepared to take 1 minute images when the bladder is full and after the patient voids
- Acquisition
- Filling (dynamic) images
- With the patient in the supine position administer the saline into the urinary bladder and start the first set of dynamic images
- As the saline starts into the bladder inject the radiopharmaceutical
- Static images - When the bladder is full take at least one or more static images
- Voiding images
- If the child is old enough sit the patient upright and place the camera behind the patient
- If it is an infant, the patient should remain in the supine position
- Release the clamp on the catheter and start the second set of dynamic images and collect the radio-saline/urine into the appropriate receptacle
- Take a one-minute post void image
- Remove the catheter
- Calculation of residual urine volume
- Measure the amount of voided urine in mL
- Draw an ROI around the full urinary bladder and label this as A
- Draw an ROI around the empty urinary bladder (post void) and label this as B
- From the above formula, place the counts identified from the ROIs drawn and enter the amount of urine volume
- Formula determines the amount of residual urine remaining the patient/LI>
https://www.studyblue.com/#flashcard/view/9667245

http://www.cmej.org.za/index.php/cmej/article/view/2792/3141