- Thoses that do not cross the BBB
- 99mTc pertechnetate (04-) with NaClO4- or KClO4- (200mg 1.5 to 8 hours prior to injection)
- 99mTc diethylenetriamine pentaacetic acid (DTPA)
- 99mTc glucoheptonate (GH)
- Those that do cross the BBB
- 99mTc d, 1-hexamethylpropyleneamine (HMPAO)
- 99mTc N, N'-1,2-ethylenedyiylbis-L-cysteine diethylester (ECD)
- 123I-iodoamphetamine (IMP) - [currently not being used in the United States, but is being used over in Europe]
- 133Xe
- PET imaging
- Most common radiopharmaceutical is 18F FDG
- Other shorter lived radiopharmaceuticals have been used when an in-house cyclotron is available
- In addition, related to brain imaging is the ability to image the cerebral spinal fluid
- 111In DTPA
- 99mTc DTPA is not recommended. This is due to the lack of possible sterility and shorter half-life
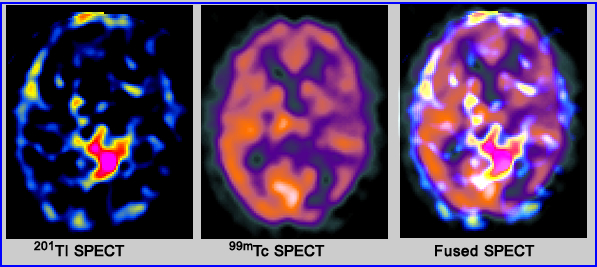
- In brain oncology (ex. glioblastomas) 201Tl-201 and 99m Tc sestamibi have been used to detect disease
- Related to infection and cancer, 67Ga has been used
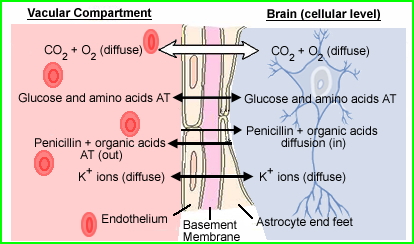
Image was modified http://137.222.110.150/calnet/Blood/page2.htm
- Controls the movement of substances to and from the vascular pool and the brain's extracellular fluid (CSF)
- Allows specific nutrients required by the Brain to pass to and from the cells within the brain
- Protects the brain from toxic chemicals
- Capillaries in the brain have tight endothelial junctions and continuous basement membrane - prevents large molecules from being absorbed by the neurons
- Astrocyte foot processes is the other component of the basement membrane and it restrict the entry of certain materials at the cellular level
- Examples of material that crosses the BBB via active transport are:
- Lipophilic substance
- Glucose
- Electrolytes
- CO2 and O2

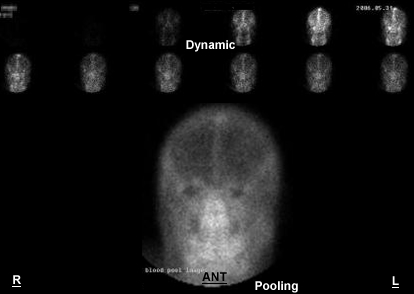
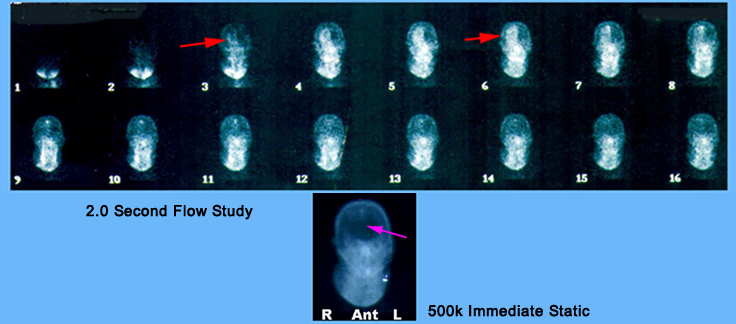
- Part I - Dynamic
- Administer
- Place the patients neck and head within the camera's FOV
- This can be done either ANT or POST (consider the possible pathology)
- Set the flow study to 2-second per frame and inject, IV bolus: 99mTc DTPA or GH or 99mTc04-
- Dynamic images are then collected for one to two minutes
- Part II - Immediate Static
- Complete an immediate static image ~500k in the same position
- If there is any abnormal pooling consider taking additional static images around the area of interest
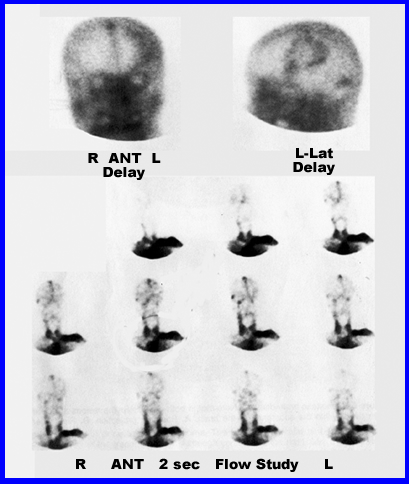
- Part III - Delayed images +++++++
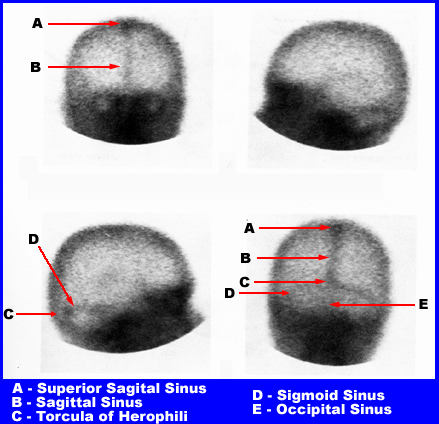
- The above images are an example of a normal brain scan with the sinuses labeled
- If pertechnetate is used, delayed imaging should be done no less than 2 hours post IV injection
- If GH or DTPA is used imaging may start at 1.5 hours (related to increased excretion of the radiopharmaceutical)
- When imaging the brain , exclude as much of the facial activity as possible (extenstive, non-essential activity is seen below the obits of the eyes)
- Take 500k images of ANT, POST, R-LAT, and L-LAT
- Vertex view is required when abnormalities are noted around the upper portion of the brain (superior sagittal sinus)
- Shield should be put around the patients shoulders
- The head must be hyper-extended off the imaging table
- The camera should be positioned in an angle that prevents activity being picked from the torso (demonstrate in class)
- If suspicious/questionable (increased) activity is seen anywhere in the brain, further delay imaging is warranted (one to two hours later)
- Lack of blood flow to the BBB will result in the lack of uptake in the area of the brain - brain death
- Delayed blood flow on the affected side is an indication of stroke - may be referred to as the flip-flop phenomom
- Increased blood flow in the dynamic phase indicates a highly vascularized area - vascular tumor or AV malformation
- On delayed images increased uptake in the brain occurs when there is damage to the BBB (examples are stroke and tumor)
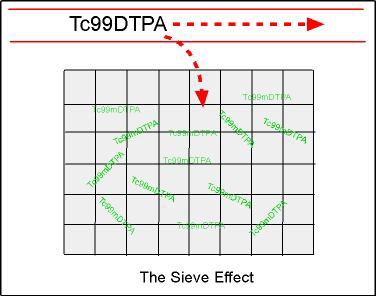
- Sieve effect - As the diagram indicates, when an area is damaged (gray area), the radiopharmaceutical becomes trapped; as trapping increases, uptake in the area can be seen
- In addition, the radiopharmaceutical is quickly excreted out of the blood via the kidneys, reducing background levels in the vascular pool and giving better target to background concentration in the damaged area of the brain
- Uptake in the choroid plexus
- If pertechnetate is used NaClO4- or KClO4- must be given
- These agents prevent radiotracer uptake in the area of the choroid plexus.
- Choroid plexus extracts plasma from the vascular pool and produces CSF. Along with the extraction of plasma, the radiotracer also becomes trapped causing activity to accumulate in this area
- If NaClO4- or KClO4- is not given, then pertechnetate (small molecule) gets trapped at the choroid plexus showing intense uptake at the site
- The above represences the four views of a delayed brain scan. These images are normal
http://surge.ods.org/xeleris/xeleris.htm
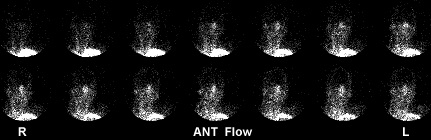
- Normal
- Activity ascends up the left and right common carotids and the vertebral arteries. The arterial flow shows bilateral symetry through its arterial and venous phases. When the superior sagittal sinus "lights up" (top/center of the head) flow enters its venous phase.
- Outline of arterial phase:
- Identifying the parts: 1 - Anterior Cerebral A., 2 - Middle Cerebral A., 3 - Internal Carotid A., 4 - Posterior Communicating A. (Part of the Circle of Willis), 5 - Posterior Cerebral A., 6 - Superior Cerebellar A., 7 - Basilar A., 8 - Anterior Inferior Cerebellar A., 9 - Vertebral A., 10 - Anterior Spinal A., 11 - Internal Carotid A., 12 - External Carotid A., 13 - Subclavian A.
- Common Carotid Artery > External Carotid Artery > Internal Carotid artery > Circle of Willis > Middle Cerebral Artery
- Vericbral Artery > Basilar Artery > (branches Superior Cerebellar A. and Posterior Cerebral A.) Circle of Willis
- Brain death
- Only needs a flow study to be confirmed postive, however, immediate are sometimes acquired
- Lack of blood flow to the brain indicates brain death
- This is caused by swelling around the base of the brain, which cuts off blood flow
- Further indication is the lack of sinus activity which means that there is no venous return
- Some scalp activity maybe noted
- Documented literature suggests the use of a tourniquet placed around the upper portion of the skull to reduce scalp activity. In my experience this does not work
- The above patient was sent to nuclear medicine for brain death evaluation. History indicated that the patient had shot himself in the head. What do the resutls of the exam indicate?
- Is there blood flow?
- Where is the blood flow? [Hint] Red arrow is the area of the penetrating bullet
- Do you see any sinuses [Hint] Purple arrow is the area of the sagittal sinus
- Do you see the superior sagittal sinus?.
- Glioblastoma (as seen above)
- Is a fast growing tumor and is highly vasularized
- It will appear hot in all three phases
- On the delay image the center of the tumor may appear cold
- Cold area is the results of necrotic tissue
- Hot circular area indicates viable tumor
- Looks like a doughnut
- Cerebral vascular accident (CVA)
- Will not be positive for at least 7 to 14 days post onset
- Flow study will be delayed on the affected side
- Referred to as the flip-flop phenomenon where the area of the brain that did not have the stroke receives the blood supply first
- On delayed images the affected side shows diffused uptake with more intense uptake along the edges of the CVA
- Brain Mets
- Flow study is negative
- Delays maybe equivical which requires further delays
- Taking a 4 hour delay is sometimes required. This will improves target to background and may inhance tumor imaging
- Abscess
- Basically cold in all three phases
- On delays, there will be hot rim of activity with a cold center
http://www.miracosta.cc.ca.us/home/lmoon/death.html


Return to the beginning of the document
Return to the Table of Contents
6/22
A Clinical Manual of Nuclear Medicine, by JM Walker and D mMargouleff. Appleton-Century-Crofts/Norwalk, CN 1984