This is part of tape series that I was involved from 1989 to 2002. One of my presentations discusses the utilization of Kinevac in hepatobiliary imaging. To me one of the BIG mistakes made in nuclear medicine has to due with the administration of Kinevac. While you will find typos and references that maybe difficult to follow, overall I think you will be able to take extract the following points:
- Advantage/disadvantage of the 3-minute infusion of kinevac
- Advantages/disadvantages of the 30 and 45-minute infusions of kinevac
- Comparison of the above protocols.
- Rationale for following strict protocols - don't vary the routine!
Application of Kinevac in Hepatobiliary Imaging
There are two reasons to inject is Kinevac in a hepatobiliary procedure and they are well know. The first, which may not be used as often, is to administer it to a patient that has been fasting for 24 hours or more. The rational here is that prolong fasting has to effect the way the gallbladder and the sphincter of Oddi functions. Prolong fasting causes the sphincter of Oddi to constrict and the gallbladder to remain relaxed and full of bile. Failure to stimulate the gallbladder may result in the radio-bile to just flow right on by the GB, never entering the cystic duct. Treating the patient with Kinevac will then relax the sphincter of Oddi and stimulate the gallbladder to contraction. So that when IDA is administered, radio-bile will enter the gallbladder as it relaxes from Kinevac stimulation. Of course it should be noted that GB visualization only occurs, if there is nothing blocking the cystic duct.
The second reason to administer Kinevac is to determine the gallbladder ejection fraction. And it is here that we will focus our attention. There are two ways in which to administer Kinevac in the literature and perhaps the more popular of the two is to administer a 0.02 ug/kg dose over a 3-minute period of time when the gallbladder is at maximum filling. Usually the gallbladder is at maximum filling between 30 to 60 post administration of IDA. The second method of Kinevac infusion is to administer the same 0.02 ug/kg dose over an extended time period, which is usually between 30 to 45 minute time. Likewise infusion starts when the gallbladder is at maximum. Before we compare and analyze these procedures let us take a look at both procedures let's first look at how Kinevac is prepared, infused, as well as how the how the EF of the GB is calculated.
A look at the protocol for the 3-minute administration of Kinevac
- Using Kinevac - The 3-minute dose
- Prepare the vial of Kinevac
- Usually a vial of Kinevac contains 5 mg (desiccated)
- Dilute with 5 mL of sterile saline (1 mg/mL)
- Prepare patient dose
- Calculate patient dose at 0.02 ug/kg of body weight
- Example of dose preparation on a 70 kg patient
- 0.02 ug/kg * 70 kg = 1.4 mg dose
- 1.4 mg divided by 1mg/1000 mL = 1.4 mL dose
- Draw up 1.4 mL into a 10 mL syringe and add 8.6 mL of sterile saline
- Connect the dose to a syringe pump
- Set the dose to be administered over 3 minutes
- Camera setup
- Collimator - LEHR
- Matrix - 256 x 256
- Acquisition - 1 minute or 700k (specific time is preferred)
- Procedure
- Collect routine images following Tc99mIDA administration (per department protocol)
- Determine when the GB is at maximum filling
- Take one additional image and label it as Pre- Kinevac dose
- If your prior acquisition is set to counts reset to preset time format
- Inject Kinevac IV over a 3 minute period of time
- Collect a post 5 minutes Kinevac dose and repeat every 5 minutes for a total of 20 minutes to 30 minutes
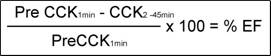
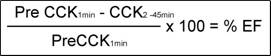
- Calculating the %EF of the GB
- Display the images

- Draw an ROI over the pre- Kinevac GB
- Draw an ROI over every other GB image that is acquired
- Plug in the numbers to the above formula to determine %EF of the GB
- If the EF of the GB is <35% chronic cholecystitis is diagnosed
- If the EF is >35% the GB is considered normal
A look at the protocol for the 45-minute infusion of Kinevac
- Using Kinevac - The 45-minute dose
- Vial of Kinevac is prepared the same (see above)
- Dose of Kinevac is the same (0.02 ug/kg)
- Assuming the patient weight is 70 kg, remove 1.4 mL solution from the Kinevac vial and add this to a 100 mL IV bag of sterile saline
- Connect the bag of sterile saline to an IV pump
- Set up to deliver 2.2 mL per minute (100 mL/45 minutes)
- Camera setup - same as the 3-minute infusion
- Pre- Kinevac Acquisition - same as the 3-minute infusion
- Acquisition protocol changes when Kinevac is administer to a dynamic 1-minute format
- Matrix - 128 or 256
- Acquisition - 1 minute images for 45 minutes
- When the gallbladder is at maximum filling start 1-minute serial images
- The first image is considered the pre- Kinevac image
- After the first minute has been collected, start Kinevac infusion
- Calculate %EF of the GB
- Display the images and draw an ROI around the gallbladder (first image)
- Calculate % EF using the following formula
- Note: the pre- Kinevac is compared to the other 44 one-minute images
- Time-activity curve may also be generated
Now let us look at the details and my first question is which procedure is better? Please note that all of the authors mentioned are reference at the end of your study guide. According to Ziessman et al there is an indication that a 30-minute infusing was preferred over the 3-minute IV injection. Several interesting points where identified as to why this was concluded, so let's look at his research. Three methods of Kinevac administration were completed on 23 normal volunteers and each method was completed on separate days. The three methods included analyzed are as follows: method 1 received a 3-min infusion of 0.02 ug/kg , method 2 received a 30-min infusion of 0.02 ug/kg, and method 3 was the same second method accept that they received 0.01 ug/kg dose infused over 30 minutes Research revealed that the 3-min infusion of Kinevac had a significantly lower EF of the GB when compared to method 2 and 3. EF on the 3-minute infusion rate was 56% at 30 minute post infusion of Kinevac where the EF from method 2, that is the 30-minute infusion rate had an EF of 70% which occurred at the end of the infusion. In addition the 3-min infusion had an exponential EF curve where the 30 minute infusion curve was linear curve.
Furthermore, six patients in method 1 had an EF of below 35% while none of 30 minute infusions had an EF that was that low. This is important when considering that many institutions diagnose gallbladder disease when the EF is at or below 35%. Note that I haven't said much about the third method, this is the one that received a 30 minute infusion of Kinevac, however, the dose was only 0.01 ug/kg dose. In this method, the article states that data was limited and details regarding the %EF were not given. However, while no specific numbers were given Ziessman did state that decreasing the dose to 0.01 ug/kg did not significantly alter the EF when compared to method 2. This data indicates that reducing the Kinevac doesn't seem to effect the EF, it’s the rate it which it is administered that effects the EF of the GB. In addition, Zeissman and colleagues concluded that the slow infusion of Kinevac was the preferred method with the rational that it was more physiological with a linear response in the ejection fraction curve and had no side effects where noted when it Kinevac was administered. Also, there was less variability and he believed that a 30 infusion of Kinevac would improve the specificity of the test.
Further development on the extended infusion time occurred with an article written by Yap and colleagues. Initially part of the study examined 40 normal volunteers where their gallbladder ejection fraction was defined by cholescintigraphy (or administration of Tc99mIDA) with a 0.02 ug/kg dose of Kinevac infusion over 45 minutes. The mean ejection fractions on these normal gallbladders were 74.5 %. From this data it was determined that anyone with an EF of greater than 40% was considered normal. Next this data was used on 103 patients that displayed symptoms of acalculous cholecystitis. Gallbladder ejection fraction procedure was completed on all 103 patients and 21 of the 103 patients had abnormal gallbladder ejection fractions. From this group of 21, 11 patients where selected for cholecystectomy and 10 where not. All patients where followed for 13 to 54 months to see if their symptoms went away. Of those that had surgery 10 of the 11 lost their symptoms. Of those that did not have surgery, all 10 continued to be symptomatic. Two of those 10 patients from the non-surgical group finally underwent gallbladder removal. Of the 13 gallbladders removed 12 showed evidence of chronic cholecystitis, muscle hypertrophy, and/or narrowing of the cystic duct. The study concluded that the 45-minute infusion of Kinevac was an acceptable and reproducible method for evaluating gallbladder injection fraction and that removal of the gallbladder from patients that have reduced ejection fractions was an acceptable method of treatment.
From our first two articles the extended infusion time for Kinevac administration seems to be the more acceptable method to determine EF of the GB. In addition, of all the articles written in the 1990s most if not all advocated the use of an extended infusion time for Kinevac for the analysis of gallbladder ejection fraction. Hence should you decide to use the an extended infusion rate for Kinevac how long should you collect the data. In this area the literature is seems to indicating that either the 30 or 45 minute infusion rate are both acceptable. Another interesting point regarding the two specific articles that I've just discussed … both articles were published one-month apart.
Now let us spend some more time looking at the 3-minute IV administration of Kinevac which I would guess is the more popular way EF of the GB is done, at least this is how all the area hospitals in the Louisville area complete this procedure. So, if this is your method for analyzing gallbladder ejection fraction, then I believe we need to spend some time on addressing several issues regarding the 3-minute infusion of Kinevac. First is the time in which the agent is infused and second is a look at what percent is really considered abnormal?
Let's take a look at time in which Kinevac is administered. The key here is that it must be administered exactly over three minutes. How often have you seen or actually done a 3-minute infusion with Kinevac with a syringe pump? From my experience this rarely occurs. I have seen the Kinevac dose administered by a resident in as little as 30 seconds. Then I have watchful technologist give what he/she thinks is an exact 3-minute dose of Kinevac, by carefully watching the clock. Yet still in both situations just mentioned neither one guarantee a specific 3-minute constant infusion rate of Kinevac. The only way to assure that this can be accomplished is with the aid of a syringe pump. Following the literature on this topic, it is very important to duplicate the protocol completed during researchers. In order to assure a 3-minute infusion rate is given at a specific flow rate in exactly three minutes, a syringe pump is the only method that will guarantee this process. So the question one has to ask, does a varying rate of Kinevac infusion change the EF of the GB.
Let's look at the literature to see if this question can be answered. Sarva et al looked at 22 patients without disease and following administration of IDA , at maximum filling of the gallbladder a 45-minute infusion of Kinevac was given at .02 ug/kg of body weight. The mean EF was 77.2% with a +/- 4.9% SD. On the same patient population Sarva administered the Kinevac dose over 1-minute, which resulted in an EF of 52.2% +/- 9.3% SD. It was also determined that doubling or halving the Kinevac dose to the patient did not change the %EF of the GB. So from this data one might conclude that changing the time in which Kinevac is infused will effective change the gallbladder ejection fraction. Also from Ziessman's article that we talked about earlier on normal volunteers the mean 3-minute infusion of Kinevac was compared to a 30-minute infusion where the EF of the GB of 56% and a 70% respectively. What seems to be the indication here is that when you significantly change the infusion time you significantly change the gallbladder ejection fraction on normal patients. Now my next point may not be statistically significant and I think I am stretching the data, but what happens if we combine Ziessman and Sarva data? That is a one-minute is an ejection fraction of 52%, 3-minute is 56%, 30-minute is 70%, and finally 45-minute is 77%. I think what is clinically significant is that longer infusion rates of Kinevac, from 1 to 3 minutes to 30 to 45 minutes does significantly alter the gallbladder contraction. What may not be clinically or statistically significant but should be pointed out is that EF of the GB does increase from 1 to 3 minutes and from 30 to 45 minutes. While the variation is slight EF does still increase. Ultimately, I think no matter how one looks at the data the most important aspect to realize is that, no mater which way you decide to analyze gallbladder contraction, stick adherence to specific protocol is essential. Because changing the infusion rate, even slightly may alter your ejection fraction results entering possible error into the procedure.
Let's take a look at one other point in this review that deals with the term standard deviation and try to determine why a 35% gallbladder ejection fraction is the cutoff for abnormal. Generally, when quantifying numbers, means, and percent means one tries to determine normal and abnormal values from a mean value which includes the incorporating standard deviations. As an example let us say that you have a mean value of 100 and the SD was +or- 10. From a statistical standpoint this means that 68% of the population would have a value of 90 to 110 (which is 1-sd). To include 90% of the population would have a value of 80 to 120 (or 2-sd), and to include 95% of the population would have a value of 70 to 130 (or 3-sd). And here in lies my confusion on the EF data. If one where to look at Ziessman's normal mean ejection fraction on the 3-minute infusion of Kinevac and apply with plus/minus 2-SD to includes 90% of the normal population what kind of values would we get? For the 3-minute infusion rate of Kinevac the normal mean was 56% with and SD of 27%. Hence, 68% of all normal's (1-sd) will have a range from 29% to 83%, 90% or all normal's 2% to 110%. Yet the cutoff used for a normal gallbladder ejection fractions usually is <35%. Using just one sd on the normal population gives us an abnormal EF 29%. You might be expecting me to give you answer on this, but I can't, accept to hypothesis that a study of a larger population should reduce SD and may in turn give us a more reliable number. Maybe I can appreciate a quote from Yap 's article where it is stated, "A gallbladder ejection fraction greater than 40% was arbitrarily (and I repeat arbitrarily) defined to be normal."
In conclusion I believe that it is imperative that no mater what your department's procedure is on determining gallbladder ejection you should: 1- strictly adhere to the procedure, 2 - understand the variability within the ejection fraction numbers, 3 - consider the protocol for a 45-minute infusion of Kinevac.
The last point is based on the fact that the response to Kinevac, using the 45-minute infusion method is linear (not exponential), better mimics actually physiology, may actually improve the specificity of the test, and finally does not cause any side effects. This is what Ziessman and colleagues concluded. The only rational that I can come up with for not following Ziessman is that the 3-minute infusion of Kinevac could cut down the camera time down to 20 minutes needed to complete the procedure. Yet is this the most logical choice?
References
Normal values for sincalide cholescintigraphy: comparison of two methods.
Ziessman HA, Muenz LR, Agarwal AK, et al.Radiology
-
-
PURPOSE: To establish normal gallbladder ejection fraction (GBEF) values for two sincalide (cholecystokinin [CCK]) infusion dose rates, 0.01 microg per kilogram of body weight infused for 3 minutes and 0.01 microg/kg infused for 60 minutes. MATERIALS AND METHODS: Twenty healthy subjects were examined. GBEFs were calculated for the 3-minute infusion and for each 15-minute interval for the 60-minute infusion. Normal values were determined by using the mean +/- 2 SDs and a more rigorous statistical analysis. RESULTS: With the 3-minute infusion, GBEFs were significantly more variable than with the 45- and 60-minute values for the 60-minute infusion (P < .01, .002). With intervals including 95% of the population, the GBEF lower normal range was 16.8% for the 3-minute infusion but 31% and 41% for the 45- and 60-minute values, respectively. GBEFs of less than 35% were noted in six (30%) of 20 healthy subjects with the 3-minute infusion but in only one with the 60-minute infusion. Hepatobiliary ultrasonography was performed in six of seven subjects with GBEF of 36% or less, and US findings in all six were normal. CONCLUSION: A 3-minute infusion of sincalide, 0.01 microg/kg, produces too variable a GBEF response to establish a clinically useful normal range. With 0.01 microg/kg infused for 60 minutes, clinically useful normal values were established at 45 and 60 minutes.
-
Acalculous biliary pain: cholecystectomy alleviates symptoms in patients with abnormal cholescintigraphy.Yap L,Wycherley AG, Morphett AD, et al.
Gastroenterology. 1991 Sep;101(3):786-93.
Abstract
-
A 45-minute infusion of an octapeptide of cholecystokinin (Kinevac; Squibb Diagnostics, New Brunswick, NJ) was used to measure the gallbladder ejection fraction during cholescintigraphy in 40 normal volunteers. Cholecystokinin cholescintigraphy was shown to be a reproducible test. The maximum mean gallbladder ejection fraction occurred 15 minutes after cholecystokinin infusion and was 74.5% +/- 1.9% (mean +/- SEM). A gallbladder ejection fraction greater than 40% (mean -3SD) was arbitrarily defined to be normal. The gallbladder ejection fraction test was then used to identify patients with acalculous biliary symptoms who may respond to cholecystectomy. A total of 103 patients was tested; 21 had abnormal gallbladder ejection fractions and were randomized into two groups, cholecystectomy or no operation. These patients were followed up symptomatically at 3-month intervals for 13-54 months (mean, 34 months). Of the 11 patients who underwent cholecystectomy, 10 (91%) lost their symptoms and 1 improved. Of the 10 patients in the group that did not undergo surgery, all continued to be symptomatic, 2 of whom requested cholecystectomy after 13 and 24 months, respectively. Of the 13 gallbladders obtained from surgery, 12 showed evidence of chronic cholecystitis, muscle hypertrophy, and/or narrowed cystic duct. A normal gallbladder ejection fraction was recorded in 82 patients, and further treatment was left to the discretion of their referring clinician. On follow-up, 50 patients were asymptomatic and 10 were symptomatic without specific treatment of the biliary tract; 14 underwent cholecystectomy, 8 of whom were asymptomatic. Pathological abnormalities were recorded in 6 of the removed gallbladders. It is concluded that the gallbladder ejection fraction obtained after a 45-minute infusion of cholecystokinin during cholescintigraphy is a reproducible measure of gallbladder emptying, and that cholecystectomy alleviates the biliary-type pain of patients with a reduced gallbladder ejection fraction.
-