- The A and P of respiration
- Pathway of air into the lungs
- Nose and mouth
- Pharynx, larynx, to the trachea
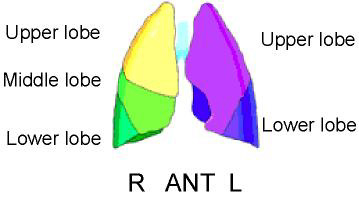
- Right and left main stem bronchi
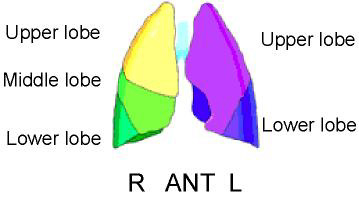
- Lobar bronchi (Upper, mid, and lower)
- Branches to terminal bronchioles (branches 16 times from trachea to t. bronchioles)
- Respiratory bronchioles (branches 4 to 7 more times)
- Alveolar duct to alveolar
- Also alveoli are also clustered in alveolar sacs
- Comments on cell structure in the lungs
- Bronchi contain cartilage in their walls (bronchioles do not)
- The entire structure contains smooth muscle, collagen, and elastic fibers that encircle the airways
- Collage and elastic fibers network throughout the lungs
- Alveoli appear in bronchioles, however, they are most abundant around alveolar sacs
- Alveoli mostly appear to have a "honeycomb" structure and are very elastic
- Alveolar type I cells allow O2 and CO2 exchange
- Alveolar type II cells are made up of surfactant and macrophages. Surfactant is defined as a lipoprotein mixture that coats the surface of the alveolar and prevents it from collapse by reducing the surface tension of pulmonary fluid.
- Surrounded by capillaries (see diagram below)
- Arterial circulation
- The pulmonary artery divides into the right and left pulmonary arteries
- Pulmonary arterials follow bronchioles
- Terminal pulmonary arteries (diameter - 35 microns) = terminal bronchiole
- Terminal pulmonary arteriole divides into approximately 1000 capillaries (diameter is 7-8 microns) surrounding the alveolar
- There are approximately 250 to 300 million alveoli in the human system
- Distance between a capillary and an alveolus is 0.05 to 0.1 μm
- Wall thickness between capillaries and alveoli is between 70 to 80 μ2
- Exchange of O2 and CO2 occurs
- Blood then returns via the pulmonary venous system (vein) to the left atrium
- Lymphatic system in the lungs
- Located in and around the lungs
- Lymphatic vessels travel to the hilum of the lung
- The lymphatic fluid drains from the lymph nodes and the mediasternum
- Generally is this is not a concern with a V/Q procedure unless there is a lot of fluid build up in the thoracic cavity (CHF)
- Breathing
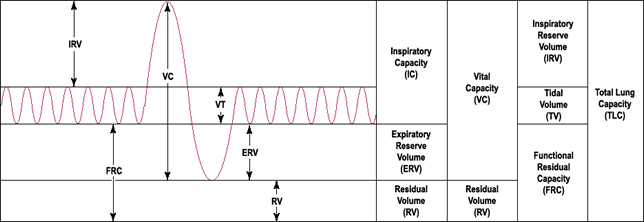
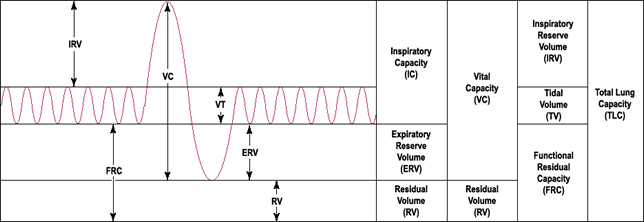
- Tidal volume is the volume of air breathed out in a normal breath
- Total lung capacity is the maximum capacity of air inhaled in the lungs
- Functional residual capacity is the amount of air left in the lungs after a normal exhalation
- Residual volume is the amount of air left in the lungs after a forced exhalation
- About 1/3 of the air does not exchange during inhalation (nose to alveoli) which is defined as anatomical dead space
- Resistance to breathing (80 to 90%) occurs in the larger bronchi and is due to turbulence caused in these large tubular areas
- The change in pressure caused by muscles results in breathing. This measurement of this exchange is defined as compliance
- Normal compliance: normal or low resistance
- High compliance: high resistance
- Closing capacity is the collapsing of the smaller bronchioles during exhalation and is resistance to airflow
- Closing capacity is greatly affected by small airway disease and COPD
- Role of gravity on the lungs
- Consider the role of gravity pulling down on the lungs where the mass of the lungs is greater at its base (should a person be in an upright position)
- Ventilation in the upright position (air exchange) is 1.5 to 2.0 greater in the upper third portion when compared to the lower third portion
- Circulation in the upright position (blood flow) increases from the apex to the base and is 3 to 5 times greater at the lung base when compared to the apex
- The role of gravity pulls down on the lungs no matter which position the lungs are in, however, it occurs to a lesser degree when the patient is in the supine position (less tissue at that angle)
- As air is exhaled, the gradient of blood flow becomes equal between the apex and base as it reaches functional residual capacity
- Ventilation to Blood flow (ratios)
- Between 2:1 to 3:1 in the upper lobes
- Approximately equal in the middle lobe
- Lower lobe circulation exceeds ventilation
- Where do most of the particles go if the patient is in the upright position and then injected 99mTcMAA? Why?
- Hemoglobin molecule contains four sites for O2 attachment
- Maximum ventilation causes all four sites on the molecule to contain O2
- When ventilation is reduced, not all the hemoglobin sites will contain O2, but will have CO2
- PO2 levels determine the amount of O2 being delivered to the patient's bloodstream
- The procedure is called arterial blood gas (ABG) test, which requires an arterial draw - link
- The normal PO2 level is between 90 - 110
- Reduced levels of PO2 relate to the lack of O2 being delivered to the alveoli (which may be due to)
- PE
- COPD
- Small airway disease
- Pneumonia
- Or anything that causes the reduction of O2 attachment to hemoglobin
- A look at disease in the lungs related to perfusion/ventilation imaging
- Single large PE - blocks blood flow but not ventilation - Perfusion will show a large cold wedge segment, and the ventilation should look normal
Perfusion Image
 |
Ventilation Image
 |
- Many PE - blocks blood flow but not ventilation - Perfusion shows several to many smaller cold wedged segments and may sometimes show a "rat bite" defect on the edges of the lung where the ventilation will look normal
Perfusion Image
 |
Ventilation Image
 |
- COPD - chronic condition affects both ventilation and perfusion - Perfusion will look normal to patchy, and the ventilation will appear patchy. The "patchy" defect is due to the absence of activity in that area of the lung. This is caused by damage to the surrounding tissue or could even be mucous plugs. In either case, the ventilation dose has difficulty in entering.
Perfusion Image
 |
Ventilation Image
 |
- Tumor: suppresses the bronchioles and smaller pulmonary arteries/arterioles - Perfusion and ventilation will usually show a similar large cold defect
Perfusion Image
 |
Ventilation Image
 |
Return to the beginning of the document
Go to the next lecture
Return to the Table of Contents
9/21