- Hepatocytes pick up the radiopharmaceutical
- Bile flows through the hepatic ducts
- To the cystic duct and into the gall bladder
- Bile flows out of the gall bladder into the common bile duct and finally into the duodenum
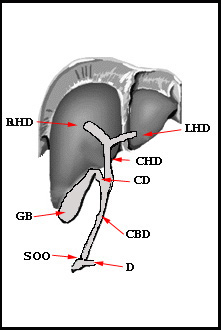 |
Right Hepatic Duct (RHD) Left Hepatic Duct (LHD) Common Hepatic Duct (CHD) Cystic Duct (CD) Gallbladder (GB) Common Bile Duct (CBD) Sphincter of Oddi (SOO) Duodenum (D) Falciform Ligament (FL) |
- 99mTc DISIDA (Disofenin) (Hepatolite)
- Example of a package insert
- In normal functioning liver 88% of this agent is excreted by the hepatic system with 10% by the kidneys
- Acceptable visualization of hepatic function can be assessed with bilirubin levels of up to 20 mg/dL
- 99mTc BROMIDA (Mebrofenin) (Choletec)
- Has the greatest hepatic uptake at ~98%
- Least affected by high levels of bilirubin
- General comments on IDA physiology
- Once injected, IDA binds to plasma protein, which reduces renal excretion
- IDA competes with bilirubin at the same sites of extraction on the hepatocyte, this type of competition is known as competitive inhibition
- The greater the level of bilirubin, the less the uptake of IDA and the greater the renal excretion
- The hepatocytes extract IDA and bilirubin via active transport
- Points that constitutes a normal scan
- Normal bile flow throughout the hepatic system
- Gall bladder fills with activity
- Activity dumps into the small intestine
- All of this occurs within the hour
- Acute cholecystitis
- Gall stone blocking the cystic duct
- Gall bladder does not image
- Small intestine visualizes
- Chronic cholecystitis
- Temporary blockage of the cystic duct
- Gall bladder appears after the 1-hour injection
- Small intestine is visualized
- Acalculous cholecystitis (vs. calculous)
- Reduced function of GB without stones
- Slug/inflammation of the gall bladder
- The gallbladder usually fills, but there is a reduction in the injection fraction when kinevac/sincalide (synthetic form of CCK) is administered
- More data on kinevac can be found at: https://www.wellrx.com/kinevac/monographs/
- Dumping of the small intestine should be seen
- Setup
- 6 - 8 mCi of IDA
- LEHR collimator
- 256 x 256 matrix
- Following IV administration
- Static acquisition
- 750k per image
- Acquire every 5 minutes
- Image for at least 60 minutes
- Dynamic acquisition (alternative)
- Take 1-minute images dynamically
- Collect data for 60 minutes
- The study is complete when
- Gal bladder visualizes
- Activity is seen in the small bowel
- Morphine augmentation (not done in the Richmond area)
- Administered when there is dumping of the tracer into the small bowel, but no activity is seen in the GB
- After one hour consider injecting morphine
- Without morphine delay images may take up to 4 hours - you need to wait for all the activity to leave the GB
- If activity is not seen in the GB after 1 hour, administer 0.04 mg/kg morphine IV for 2 to 3 minutes
- Causes constriction of the Sphincter of Oddi resulting in pressure building up within the CBD
- Continue imaging every 5 minutes for up to 30 minutes
- If GB does not visualize, then acute cholecystitis is diagnosed
- Kinevac should not be administered immediately following morphine augmentation
- If kinevac is used pre-post morphine, a 30 minute delay is suggested
- CCK derivative (Kinevac )
- Should be administered if the patient hasn't eaten for more than 24 hours
- Reason - GB stasis
- Kinevac dose = 0.02 μg/kg of body weight
- Dose patient 30 minutes before IDA injection
- Causes contractility of GB reducing a false positive study
- Should be administered if the patient hasn't eaten for more than 24 hours
- Determination of GB ejection fraction to rule out Acalculous cholecystitis