- The original scanner
- When CT was first developed its collimated x-ray beam was 3mm thick and 13mm wide. On the opposing side was a single detector which recorded the attenuated beam
- The beam would swipe across the patient, in a linear fashion, collecting the attenuated data. The data collected within the slice was referred to as a single translation
- Once the translation was acquired the x-ray tube and detector would move 1o and repeat the linear transmission collecting its second translation
- In the original scanner a single translation contained 160 rays (or x-ray beams) of data. In today's technology there are at least a 1000 rays within a single translation
- This first generation CT acquired 180 views (completing 1/2 a circle), stepping around the patient collecting data in a semicircle. This information would contained 360 degrees of data
- This process was considered slow (compared to today's technology) and would take about 6 seconds to complete
- Acquisition and reconstruction
- Remember the concept of pixels and voxels from our SPECT lectures - consider CT having a similar application
- The similarity being our ability to image 3 dimensional space, however, instead of physiological analysis, anatomical data is collected
- And instead of counting x-rays, CT evaluates the amount of attenuation that occurs with with the x-ray. The type of attenuation being evaluated is referred to as linear attenuation coefficients (:)
- The variation in : occurs when tissue densities vary within the 3D space
- As a general rule, a CT matrix size is 512 x 512 with a thickness of 0.5mm2. Adding the third dimension turns the pixel to a voxel. The size of voxel is usually 1mm
- Once the data is acquired in the matrix it is usually referred to as a reconstruction matrix
- Image matrix is then interpolated from the reconstruction matrix, where display adjustments are applied, such as zoom and/or filters
- Generating the reconstruction matrix
- No is the production of the x-ray where it travels through 3D space (example above shows 10 pixels)
- Depending of the amount of density encounters there will be a variation in the ray's attenuation. This values of attenuation is referred to as :i where the beam may encounter different degrees of attenuation with a certain volume of pixels. The end point of the attenuated ray is then referred to Ni were the detector records the amount of attenuation, referred to as the linear attenuation coefficient
- Given the chart above different attenuation coefficients are displayed. These attenuations are based on a 100 kVp beam. It should be further appreciated that a typical CT tube generates a poly-energenic beam within the 100kVp . This variation is approximately 1%. Furthermore, in CT you can adjust your x-ray beam that may be as low as 70 keV and as high as 140 keV
- The attenuated sum (E:) occurs after the initial ray No passes through a set of voxels which in turn becomes No and can written as E:i = _ ln(Ni/No). In addition :i represents the amount of voxels within the ray and because it is 3D becomes wi:i, where w stands for width.
- Hence the attenuated ray is the sum of only 1 ray traveling across a set of voxels in 3D space. There are 160 ray that makes up 1 translation and 180 translations makes up one axial acquisition
- While a CT scanner calibrates its linear attenuation coefficients by initially "cutting air" via a QC procedure the "magical" number/value is water. Why?
- How does a CT scanner determine the : values in 3 dimensional space? To simplify the process let us look at a 2 x 2 matrix using an iterative alogrithmic approach, Algebraic Reconstruction Technique (ART)
- The attenuation in these 4 pixels are hypothetically unknown, however, when you apply an x-ray beam to them, No, at six different angles, 6 Ni, the values are detected (N1-6). This has been demonstrated above
- To find the : values we first sum both rays at 0 degrees. N1-2 rays have the same summation 11. Because there are 2 pixels within each ray the sum is divided by 2 making 5.5 the attenuation value for N1 and N2. This is placed into all four pixel.
- To find the : at 90 degrees ray N3 summation is 12 which is then subtracted by sum of N1 (11) and divided by its 2 pixels. The value is +0.5 which tells us to add 0.5 to each pixel in the N3 ray. The same process is applied the other ray N4, with the final value being -0.5. We now subtract 0.5 in the 2 pixels that compose the N4 ray
- At 135 degrees N5 ray sum 9 and when subtracted from the N1 it becomes -2. Because there are 2 pixels in the ray this value is divided by 2 has a difference of -1.0. We then subtract 1 from each pixel within that ray
- AT 235 degrees N6 has a final value of +1.0 which tells us to add 1 point to each pixel within that ray.
- The end result shows us that the ART method can correctly determine attenuation values
- Now imagine if you will,, these calculations being applied with a 512 by 512 matrix in 3 dimensional space

- Backprojection (Remember FBP?)
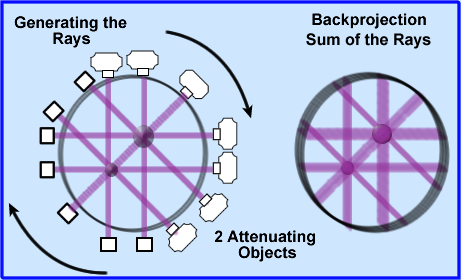
- Once the attenuated values are determined these coefficients must be backprojected, as in a SPECT image, however, instead of counts CT uses attenuated x-rays
- These attenuated values are displayed evenly across each backprojected ray, 180 around the patient
- Looking at the above image 2 attenuated objects have been placed in the volume. The image to the left is shows x-rays being projected and detected. The image on the right are the backprojected rays
- Backprojection causes the image to be blurry (just like SPECT) and therefore image filtering must be done.
- Blurriness can also be caused by something known as quantum mottle which occurs when there are too few x-rays/pixel. This causes image graininess via increased noise (sound familiar?)
- Think x-rays/pixel (counts/pixel) and then associate square root of the attenuated x-rays (square root of recorded gamma counts). The fewer the rays the greater the noise
- Spatial resolution is improved by image filtering because it reduce noise and improves contrast. On a similar thought low contrast structures that have too much noise may cause the lost of recognizable data
- Windowing
- The gray scale adjustment
- Linear attenuation coefficients can be related to another term known as Housfield Units (HU). These units vary from -1000 to 1000, with water having the value of 0. Once : is determined HU values can be calculated from the above formula. This is how the gray scale on the final image. Several : are noted above with their respective HU values. The formula can also be used to convert from : to HU
- Windowing sets the gray scale in a CT image
- Remember there is a total of 2000 HU, but only 256 shades of gray. If you wanted to look the entire HU scale via its gray scale application that mean 4 HUs would equal 1 shade of gray. Therefore slight changes in density, via the initial invasion of disease could be missed
- Therefore, the concept of windowing is applied, in which HU only looks at a small variation within the attenuation range. This allows shade of gray of to be more affective in finding small variations in density
- The following is an example for adjusting the window level and width
- When the operator selects the a specific tissue type that sets the window level at the midpoint of the HU and gray scale
- Selecting the right window becomes critical in finding disease in different structures of the body. Consider brain vs. bone and note the degree of density between both organs
- In the display above the window level/width are set to differentiate between water, fat, and muscle. Anything above an HU of 50 is going to be white while anything below -100 will be black. Should something appear above or below window width there will not be enough contrast to visual it. However, any variation between the selected HUs will have will have 254 levels of contrast/gray (256 - 2 black/white)
- One other comment noted in the literature: selecting the window width defines the amount of contrast and is referred to the "gray-scale rendition of specified tissue."


- In the literature CT development is usually referred to as 2nd, 3rd, 4th, generation, however, for our limited review, I will look at how CT scanning improved over time. The key to most of CT development is to reduced scanning time and to allow for the evaluation of a more dynamic model
- Single narrow beam with a detector evolved to three beams/three detectors on the same gantry. However, anything additional tubes/detectors created too much gantry motion
- Thin beam became fan beam which encompassed the entire patient's width. Thus further reducing the scanning time by increasing the imaging area so that the entire diameter of the patient was covered in one translation. In addition, fixed detectors were set at 360 degrees around the scanner, so that only the x-ray tube moved
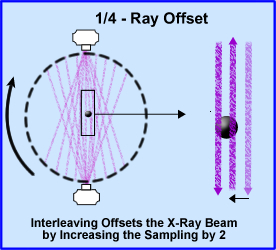
- 1/4 - ray offset takes the concept of doubling your sampling size by increasing the amount of x-rays going through the object by two. In addition the scanner rotated 360 degrees around the patient. The diagram shows beams sampling of a round the object. The second beam samples the object at 1/2 the distance from the opposite direction, hence interleaving the object and improving image resolution
- Reducing the time an x-ray goes through the patient by increasing speed and energy of the x-ray tube allowed CT analysis of the myocardium
- Slip Ring and Helical CT - In prior technology cables limit the rotation of the gantry. The scanner could spin in one direction, but then have to de-spin so it can spin again. By using a drum, grooves with metal brushes to "connect" the electricity, cables were no longer required allowing the CT scanner spin in either director without having to unravel itself. Additionally, the scanner would spin in a spiral pattern, never overlap.
- Helical pitch is used to define the table movement per rotation divided by the slices thickness
- Example: If slice thickness is 5mm and the table moves 5mm per rotation then this equal 1.0
- Hence a pitch of 1.0 with no under or over over sampling
- If you go beyond a pitch on1.0 then areas become under sampled and estimations of their : values must be made
- If the table moves too fast then there may be an motion artifact

- Technical points
to remember
- CT uses a beam that generated around 100 to 140kVp = 100 to 140keV
- Beam hardening occurs when an x-ray beam has to penetrate deeply into an object. The more density it has the greater the Compton and Photoelectric effect. This causes the center of this object to be darker because fewer x-rays are recorded. A similar concept in SPECT is referred to as cupping
- Septas are used in CT and are placed between detectors. This reduces scatter of the attenuated beam and improves contrast
- Quantum mottle and a low count image in nuclear are similar concepts
The Beginning of the Document
Next Lecture - PET/CT Imaging Artifacts
Return to the Table of Content
Most of this this lecture came from the following articlePrinciples of CT and CT Technology by Lee W. Goldman, Journal of Nuclear Medicine Technology Volume 35, Number 3, 2007 115-128