- This nuclear medicine procedure is done to evaluate resectability of lung tissue on patients with lung carcinoma or lung transplant
- The concern relates to whether or not there is enough viable lung tissue following the removal of cancerous lung tissue
- The rationale to perform the thoracotomy is based on:
- Resecting the tumor
- Patient's ability to tolerate the surgical results
- It should also be noted that a split lung procedure is very non-specific in finding lung cancer and it is unable to identify metastatic involvement
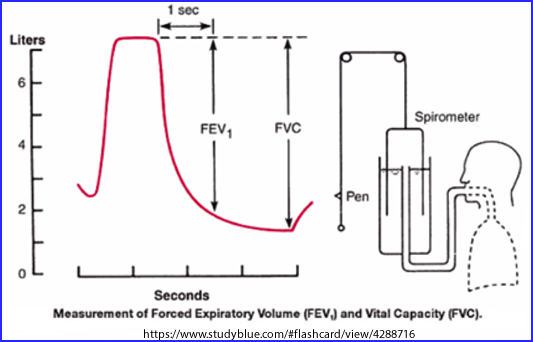
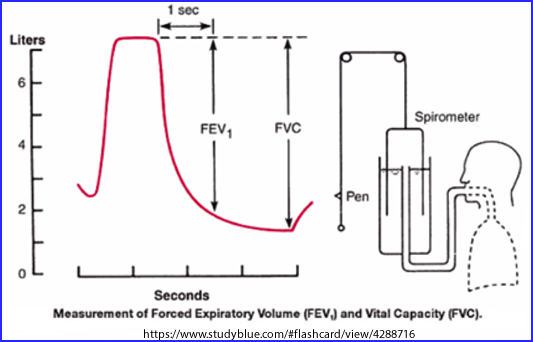
- The study is combined with pulmonary lung function test
- Forced expiratory volume in time (1 - 3 seconds) - FEV1
- Forced vital capacity (FVC) - volume of air forced out of lung
- Study should be done when the patient is not on a bronchodilator
- Why is a bronchodilator NOT recommended?
- The patient can tolerate significant amount of lung removal if the pulmonary lung function test meets the following values:
- FEV1 is greater than 50% of the FVC and the FVC is greater than 2 L
- Maximum voluntary ventilation is greater than 50% of the predicted value
- Ratio of residual volume to total lung capacity is less than 50%
- Surgery is usually not performed if the FEV1is below 0.8 L
- When the above criteria is/are not met, a split lung procedure using 99mTcMAA is usually ordered (Note: 2 a-c)
- The procedure is as follows:
- Inject the patient with 4 mCi IV using 99mTcMAA
- Camera setup
- 256 x 256
- LEHR collimator
- 500 to 750k counts per image
- Take anterior and posterior images
- Once the images are collected, ROIs are drawn over the R and L lungs (refer to image)

- Counts are then determined
- Anterior R lung and posterior R lung counts are summed
- Posterior R lung and posterior L lung counts are summed
- Average counts from each lung are then determined (R and L)
- Geometric or arithmetic mean maybe used (arithmetic is used in the example)
- Ratio for L lung to R lung is determined (see image)
- From a nuclear medicine technologist's standpoint, the study is complete.
- What does the physician do with these numbers?
- Following a pulmonary function test the preoperative FEV1 value is determined
- In the example 2200 mL is used
- The preoperative value is then multiplied by ratio of R lung counts, since this is the lung that has no disease.
- The assumption is that there may be additional disease in the L lung, and that all of the L lung may be removed during surgery
- -- This is the more conservative approach --
- The postoperative predicted value is then determined and an estimation of total lung capacity is estimated (in the example used the value is 1320 L)
- Based on these calculations is surgical intervention recommended?
- Other approaches to the split lung procedures:
- Ventilation and perfusion may be used together for a more accurate approach
- Analysis of activity in each lobe may also be considered
- Lung counts are divided into each lung's separate lobes; that is, as opposed to counting each whole lung.
- The right side would have 3 regions and left side would have 2 regions
- The same approach is used to determine counts and ratios; however, it is done at the lobular level
- Literature suggests that these other applications do not improve the patient outcome, post surgery
Return to the beginning of the document
Return to the Table of Content
Reference - http://www.meddean.luc.edu/lumen/MedEd/medicine/pulmonar/lungca/man-preo.htm
End of Lung Lecture - Review Study Guide
10/22