Lymphoid organs and tissues may be classified according
to functions and organization as follows:
I.
PRIMARY LT:
THE THYMUS - is a primary lymphoid organ, because
it seeds, populates, secondary lymphoid organs with T
lymphocytes; Readings:
Junqueira, Basic Histology, CH 14, p.273-8, Thymus.
A. CHARACTERISTICS:
1. LOCATION:
A broad flat bilobed organ, located beneath the upper sternum in the
anterior mediastinum.
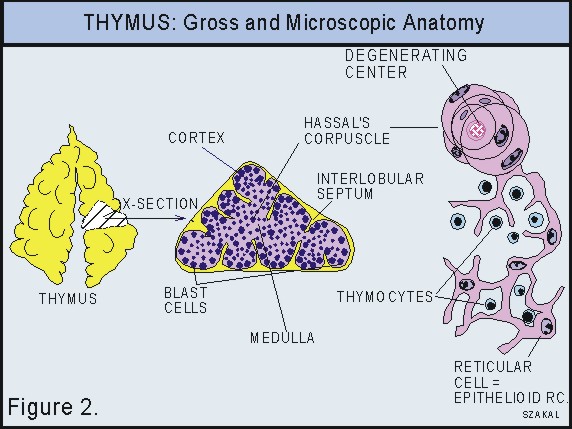
2. ORGANIZATION:
Highly organized, but different in several aspects from the structural
evolution shown by the secondary organs. Have: Capsule
of thin loose FECT; Septa divide it into many lobules,
Vertical trabeculae; Cortex of small
lymphocytes (thymocytes), Medulla of predominantly
'reticular' cells and some thymocytes (See Figure
2.).
3. STROMA:
'Reticular' cells forming a supporting reticulum. Derived
from a paired outgrowth of the endodermal lining of the 3rd
branchial pouch of the embryo, (thus epithelial origin).These
cells are epithelioid in character, do not produce reticular fibers,
but elaborate the hormone called Thymosin (lymphoproliferative).
Blood capillary arcades in cortex.
The reticular cell layer covering the capillary arcades makes up the
"blood-thymus barrier." Nerves: from vagus
and sympathetic nerves.
4. PARENCHYMA:
Cells: thymocytes; derived from yolk sac
and postnatally from the bone marrow. They migrate to the thymus
and form blast cells (lymphoblasts, medium size lymphocytes) adjacent
to the capsule. They proliferate become small lymphocytes (thymocytes)
and migrate to the medulla. Some macrophages and eosinophils are also
present. Since reticular cells are epithelioid, the whole organ is sometimes
considered to be parenchymal.
5.
DIAGNOSTIC FEATURES: Lobulation, lack of lymphoid nodules,
Hassal's corpuscles (believed to be dying epithelioid
'reticular' cells);
|
B.
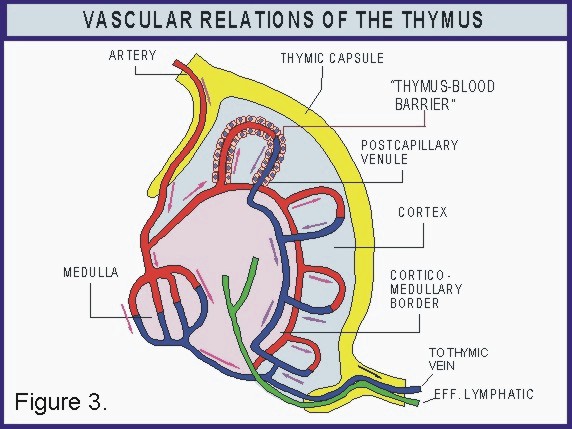
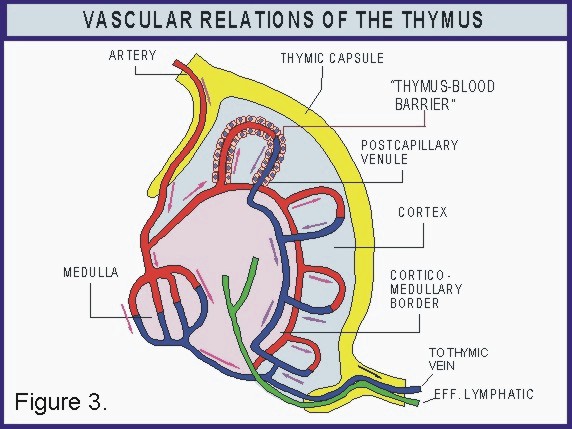
LYMPHATIC and BLOOD SUPPLY (See Fig.
3).
1.
Arteries enter the thymus through the septa
between lobules; They branch; Some arterioles course along the
cortico-medullary border and supply blood primarily to the cortex
via arcades of anastomosing capillaries
which join postcapillary venules.
2. The capillary arcades are tightly covered on the outside
with a layer of epithelioid reticular cells. This layer and
some surrounding macrophages form the "blood - thymus
barrier" which keeps foreign antigenic material from
entering the cortex and keeps developing T cells from being
exposed prematurely to foreign antigens.
3.
Another branch enters the medulla. It gives rise to fenestrated
capillaries. The postcapillary venules allow entrance of thymocytes
coming from the cortex to enter the circulation and be transported
to secondary lymphoid organs.
4.
Veins and efferent lymphatics leave the
thymus via the septa. Veins drain to the
thymic vein .
|
 |
|
C.
FUNCTIONAL CONSIDERATIONS:
1.
The THYMUS provides thymocytes which migrate to other
lymphoid tissues and
organs and function as helper cells in the
humoral or cell mediated immune response;
Also provides thymocytes which are responsible for the cell
mediated immune response;
3.
"Epithelioid reticular" cells produce thymosin
which induces proliferation and differentiation
of T lymphocyte precursors to immunocompetent (functioning)
T cells.
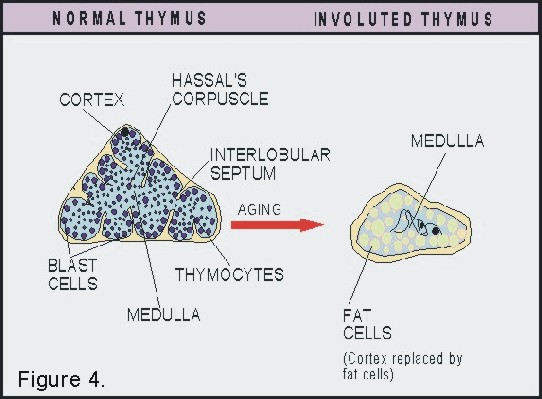
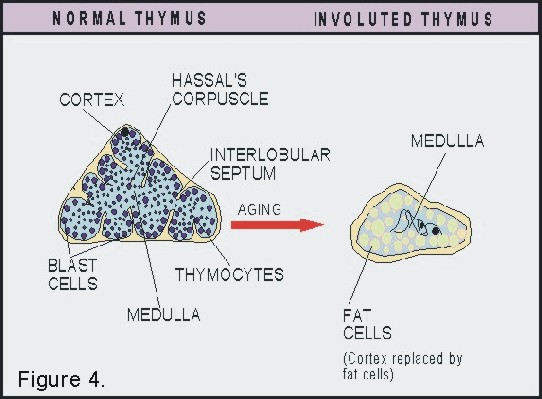
4.
The thymus becomes functionally dormant with age and involution
begins at puberty. Most of the parenchyma is
replaced by adipose tissue and the medulla
becomes fibrous. See Figure 4.
|
 |
********************************************************************************
Virtual Slides: 37 and 91. THE THYMUS:
Study the virtual slides and the digital Histology CD.
At
low magnification study the organization of the thymus. Identify
the L-FECT capsule, trabeculae, lobules, cortex and
medulla. Lobules are separated from one another
by interlobular C.T. The medulla of one lobule is continuous with
that of the adjacent lobule. Why does this appear not to be true
for all lobules in your section? Identify, Hassal's corpuscles
in the medulla. What cell types are they made of?
Under
medium and high magnification study the cortex and the medulla.
Identify thymocytes (small lymphocytes) and blast
cells located immediately adjacent to the capsule (look
like large lymphocytes). What is the significance of blast cells
near the capsule and thymocytes further away from the capsule? Where
do the precursors of the blast cells come from originally?
Identify the
'reticular cells' (epithelioid cells) forming the
stroma. Do these cells produce reticular fibers?
Why are they referred to as epithelioid cells? Where is the general
location of the thymus-blood barrier? Where do
lymphocytes go from the medulla?
*********************************************************************************
|
|
|
II. SECONDARY
TISSUES AND ORGANS
A.
Diffuse Lymphoid Tissues
1.
LOCATION: Lamina propria of mucous membranes
in the alimentary and respiratory tracts.
2. ORGANIZATION: No special organization; they are lymphocytic
infiltrations of the C.T. of mucous membranes.
3.
STROMA: Loose FECT: local blood and lymph
capillaries and nerve fibers.
4.
PARENCHYMA: Lymphocytes (mostly small), plasma cells, some
macrophages and eosinophils.
5.
DIAGNOSTIC FEATURES: Location (mucosa)
and the diffuse accumulation of lymphocytes.
 |
***********************************************************************************
LABORATORY EXERCISE:
Virtual
SLIDE 61. Search for Colon, normal. Among the crypts of Liberkuhn
in the lamina propria you will see a relatively dense presence of
lymphocytes, these represent a diffuse infiltration. Among the lymphocytes
macrophages and some plasmacells are present but may be difficult
to see them. What kind of immunologic response does diffues lymphoid
tissue represent? Humoral? Cell Mediated? Why?
Virtual SLIDEVirtual SLIDE 01, Vocal cords. Note the
diffuse lymphoid tissue among the glands in the lamina propria.
|
Virtual
slide 118. Mammary gland, active. - Diffuse
leukocytic infiltration is present around the secretory units of
the gland. Why? Identify lymphocytes, and plasma cells
(larger cells with faint, abundant cytoplasm).
************************************************************************************
|
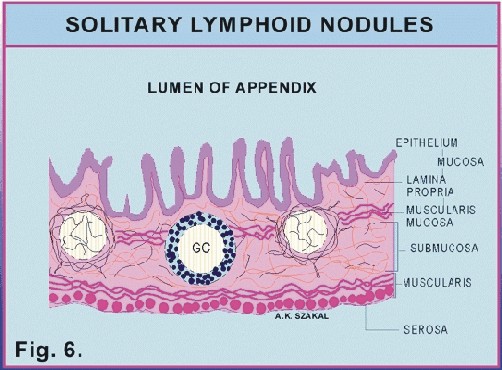
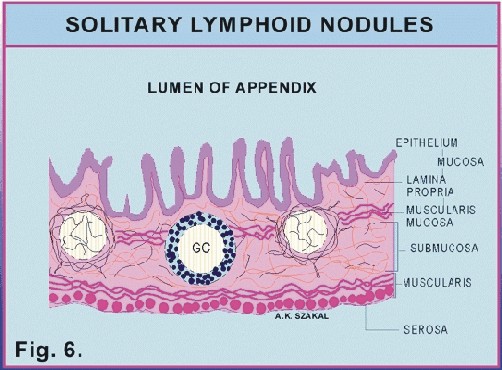
B.
Solitary Lymph Nodules
1. LOCATION: Mucosa of intestinal tract (e.g. most conspicuous
in the vermiform appendix);
2. ORGANIZATION: Organized into spherical nodules (often
called primary lymphoid follicles) of lymphocytes;
3. STROMA: Loose FECT and reticular cells (mesodermal
origin); Some reticular fibers; local blood and lymph capillaries
and nerves;
4. PARENCHYMA: Small lymphocytes, which may form a cortex
(the periphery) for the nodule; and Medium to large lymphocytes
may form a germinal center in the nodule;
5.
DIAGNOSTIC FEATURES: The isolation
(individual, not tightly grouped) of lymphoid nodules. See Figure
6.
 |
********************************************************************************
LABORATORY
EXERCISE:
Virtual SLIDE
62.
Search the data base for normal Appendix. - Diffuse
and nodular lymphatic tissue is present. Identify secondary
nodules. What is a secondary lymphoid nodule? What does
it have in its center? What is a germinal center? What is the
crown or mantle or cortex (these terms refer to the same structure)
of a secondary lymphoid nodule? Why is the dark area of the G.C.
Dark? Identify these areas!
Also use the Digital Histology CD.
*******************************************************************************
|
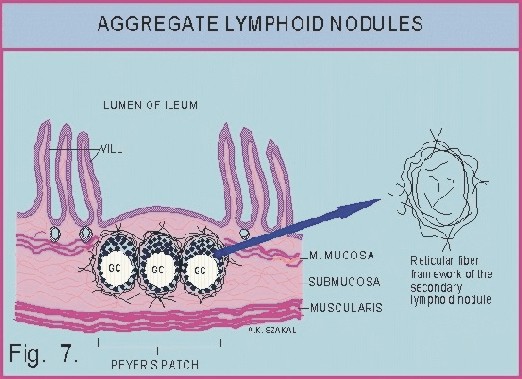
C.
Aggregate Nodules (called Peyer's
Patches)
1. LOCATION: Lamina propria
of ileum;
2. ORGANIZATION:
These are oval groups of closely associated 'pear' shaped lymphoid
nodules with germinal centers; Not bound by a
capsule; Their luminal surface is bordered by the simple columnar
epithelium of the ileum; villi are absent over Peyer's patches;
3. STROMA: Reticular
cell framework (mesodermal origin); Produce reticular
fibers, which are condensed at the periphery of nodules. Local
blood and lymph capillaries and nerve fibers.
4. PARENCHYMA: Small
lymphocytes form the periphery of each nodule;
and medium to large lymphocytes form the germinal
centers;
5.
DIAGNOSTIC FEATURES:
Organization of nodules into groups (aggregates). See
Fig. 7.
********************************************************************************
Virtual
SLIDE 58 and 59. Duodenum and Ileum - Identify
diffuse leukocytic infiltration in the lamina propria. Aggregates
of lymphoid nodules in this tissue represent Peyer's patches.
Are primary or secondary nodules present? Distinguish between
fibroblasts of the supportive stroma and lymphocytes
around the lymphoid nodules in the diffuse lymphoid tissue.
Also see the Digital Histology CD on Peyer's patches.
*********************************************************************************
D. Tonsils
1. LOCATION: At
the entrance of the throat between two arching folds of the pharynx
(e.g. Palantine tonsil);
2. ORGANIZATION: Show
an increased organization: Incomplete capsule
of compact FECT; Septa of C.T. divide the organ
into lobules; Crypts
penetrate the lymphoid tissue (10-20 crypts per tonsil);
3. STROMA: Coarse internal
framework of reticular cells (mesodermal origin)
and reticular fibers; Reticular fibers are continuous with fibers
of septa and capsule; Local blood and
lymph vessels, and nerves;
4. PARENCHYMA: A dense
sheet of lymphoid tissue parenchyma bordered by moist stratified
squamous epithelium of crypts and below by incomplete
C.T. capsule; contains a single layer of lymphoid nodules
(each with cap of small lymphocytes and a germinal center);
5. DIAGNOSTIC
FEATURES: Presence of crypts and incomplete
capsule; See Figure 8.
 |
*********************************************************************************
LABORATORY
EXERCISE:
Virtual SLIDE 38. Palatine
tonsil - A dense connective tissue capsule
is present at the base of this section (see CD) and septa
extend into the tonsil. Identify these structures! Many lymphatic
nodules are present, distinguish between primary
and secondary nodules. Diffuse infiltration
of the connective tissue is present between the nodules, and lymphocytic
infiltration into the moist stratified squamous epithelium
makes the base of the epithelium hard to define. Identify "light"
and "dark" regions of GC. In which of these areas
would you find antigen? What is the cap or crown
of a germinal center? Cap is the same os the crown or mantle;
Called cap sometimes because it looks like a cap. Are the cells
smaller in the crown or cap than in the "dark" region of a GC?
Why? See also the CD. *********************************************************************************
E.
Mucosal immunity and the production of secretory IgA
1. IgA dimers
(MW: 400,000) form the major specific humoral defense mechanism
on mucosal surfaces.
2. Some IgA in the
monomeric form can also be found in the circulation.
3. Secretory
IgA (458,000) is present in saliva, nasal mucus, bronchial
secretions, mucus of small intestines, tears etc.; It is secreted
by mucosal plasma cells as monomers and dimers.
The secretory piece (protein, MW. 58,000; not an immunoglobulin)
is synthesized by epithelial cells and it is added to the dimer.
Via the secretory piece and vacuoles the dimers are transported
to the surface of the epithelium where they are free to react
with the appropriate antigens of microbes. See Figure 8 below:
|
|